
Women who get routine cervical cancer screenings are less likely to get or die of the disease, and there are now more options for what types of screening they can choose than ever before.
New guidelines, published Tuesday in the journal JAMA, include more test options and longer intervals between those tests for women over 30. The recommendations, from the US Preventive Services Task Force (USPSTF), were last updated in 2012.
Cervical cancer was once one of the leading causes of cancer deaths in women in the US, but the number of deaths has declined substantially since routine screenings were introduced in the 1950s.
And those numbers continue to decline with additional tests and treatments. The number of deaths due to cervical cancer dropped from 2.8 to 2.3 deaths per 100,000 women between 2000 and 2015.
The cervix is the lower, narrow end of the uterus that connects it to the vagina. When cancer develops in the cervix, it is almost always due to infection with a common sexually transmitted virus called human papillomavirus (HPV). Most people who are infected with HPV clear the virus without any treatment or problems, but persistent infections with certain high-risk types can damage cells, leading to cancer.
These high-risk HPV infections can mostly be prevented with a vaccine introduced in the US in 2006, which is available and recommended for both boys and girls. But if cancerous changes do develop in the cervix, they are highly treatable if caught early with routine screening.
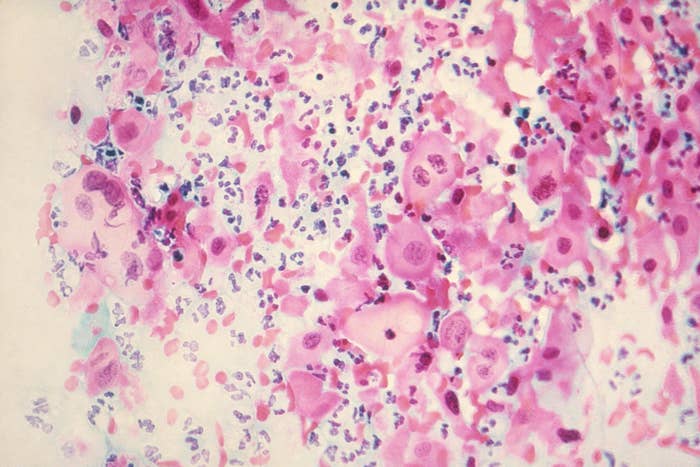
There are two types of tests used to screen for cervical cancer: cervical cytology, also known as a Pap test or Pap smear, and high-risk HPV or hrHPV testing. These can be done separately or in combination by swabbing the cervix during a pelvic exam conducted by an OB-GYN.
A Pap smear can detect cancer, or abnormal cells or tissues that may progress into cervical cancer if left untreated. The hrHPV test detects the presence of certain high-risk types of HPV known to cause cancer. Both methods have been shown to be effective at identifying people at high risk of developing cancer.
In the past, the yearly Pap smear was the standard. But things have changed. Here is an overview of the new screening guidelines:
* Women ages 21–29 should get a Pap smear every three years.
* Women ages 30–65 should get either: a Pap smear every three years, HPV testing every five years, or a combination of Pap smear and HPV testing every five years.
* No screenings for women under 21.
* No screenings for women over 65 who have had previous routing testing and aren’t at high risk for cervical cancer.
* No screenings for women who have had a hysterectomy and do not have a history of cervical cancer or precancerous lesions.
The biggest change is that women over 30 can get HPV testing alone instead of a Pap smear and that they only need to be screened once every five years if they have both tests, instead of every three. For women ages 21 to 29, the guidelines haven’t changed and Pap smears are still the gold standard.
“We have new studies that provide strong evidence that the HPV test alone is a very effective and a reasonable alternative to getting the Pap test or combination testing ... women [over 30] now have three choices that are very effective,” Dr. Douglas Owens, vice chair of the USPSTF and professor of medicine at Stanford University, told BuzzFeed News.

The new screening recommendations mean that women over 30 can choose a testing method based on their preferences or what’s available — which may vary depending on the health care provider and their resources.
HPV testing alone is not always available everywhere, Owens explained, which is one reason why the recommendations now include three choices for women. “No matter where a woman receives care, there are options for her to get a cervical cancer screening,” Owens said.
Even if you received the HPV vaccine, you still need to be screened routinely — the guidelines apply to both women who are vaccinated and unvaccinated. In any case, you should always talk to your doctor if you have questions or want to explore your options.
“Most cases of cervical cancer that occur now are in women who haven’t been regularly screened or appropriately treated ... it’s a very important preventive health service all women should receive,” Owens said.
