
The number of women getting smear tests at sexual health clinics has more than halved over the past five years, a report reveals, as government funding cuts leave councils struggling to provide a range of vital services.
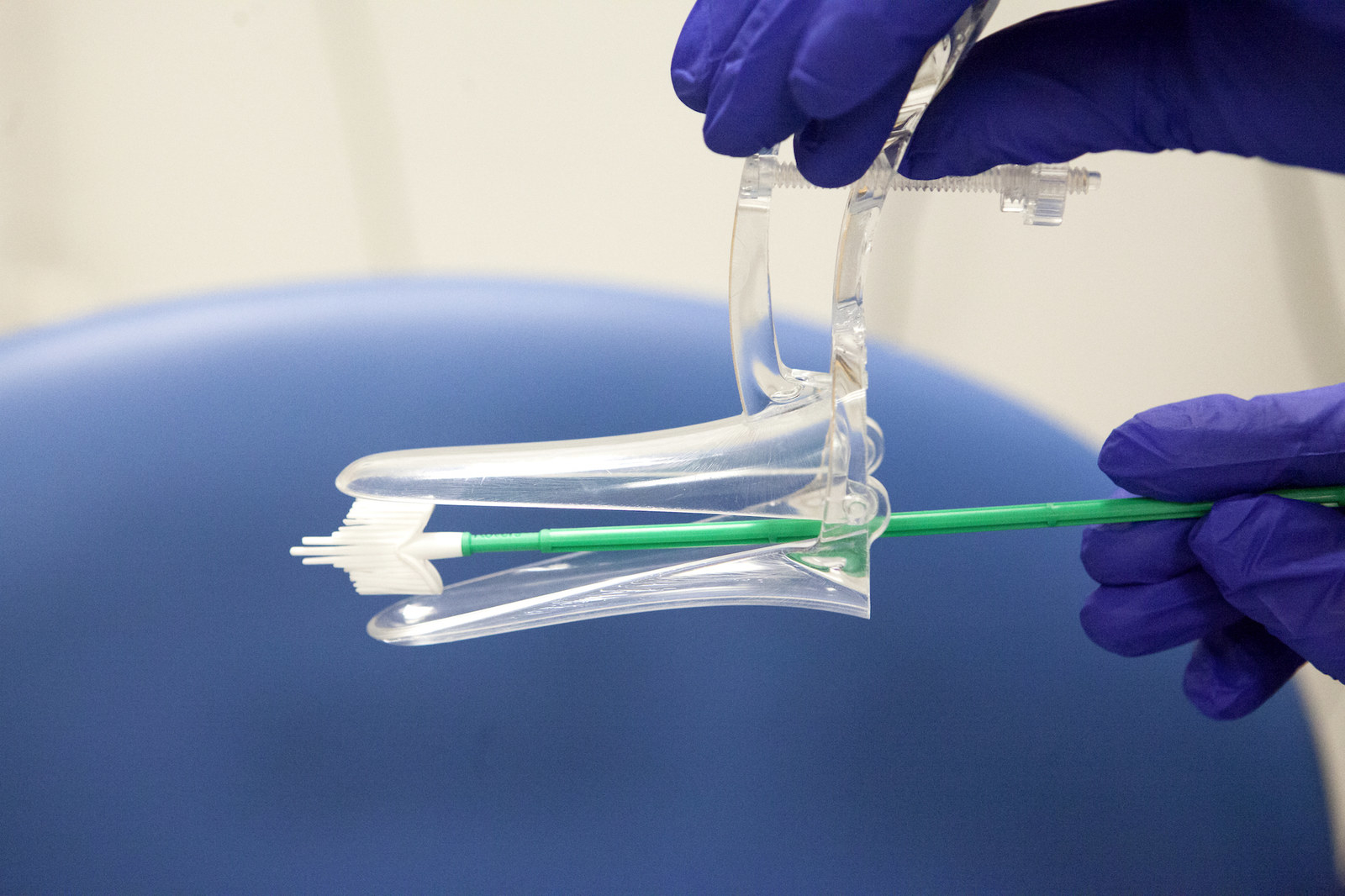
New figures from Jo's Cervical Cancer Trust show a 52% fall in women in England receiving cervical screenings at sexual health and community clinics, from 117,028 to 56,347. Wales has seen a decline of 42%, from 10,254 to 6,002.
Smear tests are just one of many services that councils have been forced to roll back following cuts of £600 million to public health funding between 2015 and 2020.
Sexual health services have suffered a 5% cut amounting to £30 million, according to the Faculty of Sexual and Reproductive Healthcare (FSRH) citing the King's Fund health charity, which has led to a sharp decline in services ranging from smear tests to provision of long-term and emergency contraceptives as well as STI checks.
At least 32 local authorities closed contraceptive services between 2016 and 2017, the Advisory Group on Contraception found, compared with 12 in the previous financial year.
Sexual health clinics often appeal to women more than GPs because they have traditionally offered a range of services in one place, allow walk-in appointments, have shorter waiting times, and do not require registration.
Dr Anne Connolly, vice president of the FSRH, told BuzzFeed News that they provide a "holistic approach" to women's healthcare provision.
"Women like choice. They like to be able to access services in one place," she said.

Because clinics are not legally obliged to offer the screenings, smear tests have been one of the casualties of the cuts.
It is a particularly concerning consequence because, statistically, women who take smear tests through sexual health services are at greater risk of cervical cancer than those who go to their GPs. According to NHS data in England 11.5% of tests taken in sexual health clinics come back as abnormal, compared with 5.9% of samples taken at a GP.
It is also worrying because the reduction of services in clinics has put more pressure on GP practices, as they pick up the slack. Every year around 5 million women are invited to screenings, with women aged 25–49 invited every three years.
Today's report found that already 7.4% of women were told no appointments at their GP practice were available when they tried to book. Channelling this high demand to GPs is likely to cause further problems.
Connolly said that reduced access to services in clinics has been the most damaging impact of cuts to local authorities' public health grants, and has exacerbated regional inequalities.
"Some women want to attend a single-sex family planning clinic because that is culturally better for them. Reducing access adds [social, financial, and cultural] hurdles to women who are most vulnerable — increasing inequalities," she said.
Jo's Cervical Cancer Trust is calling on the government to conduct an urgent review in order to identify the problems and address inequalities. It wants a national budget for cervical screening in sexual health services in England, and more GP appointments to be made available so that women will have to wait no longer than four weeks.
Robert Music, the charity's chief executive, said: "We know that we can make cervical cancer a disease of the past but we won’t get there if cervical screening attendance continues to fall."
Izzi Seccombe, chair of the Local Government Association’s community wellbeing board, stressed that women should be able to access live-saving tests wherever they live.
"The report rightly highlights the financial challenges that Clinical Commissioning Groups, GPs, and council-commissioned sexual health services are under," she said. "We repeat our call for national government to reverse cuts to the public health grant and invest in preventative services such as cervical cancer screening to help improve attendance rates and address inequalities in accessing them.”
Jo's Cervical Cancer Trust also wants funding for pilots of self-sampling, so that women can take the test themselves — something Connolly, too, advocates.
She said the government must improve the current situation before the clinicians in sexual and reproductive health service "lose their skills" altogether, leading to more retraining costs in the future.
