
When I decided to freeze my eggs this September, it was — unlike most big life decisions I’ve made — motivated by detached practicality. After a year of unsuccessfully trying to get pregnant, I turned 35 and sat with the question of whether I was really ready to have kids. In many ways, freezing my eggs seemed like a neutral action in a sea of distressing ones: I felt that I was merely putting the question on ice while I took time to sort through some other emotions.
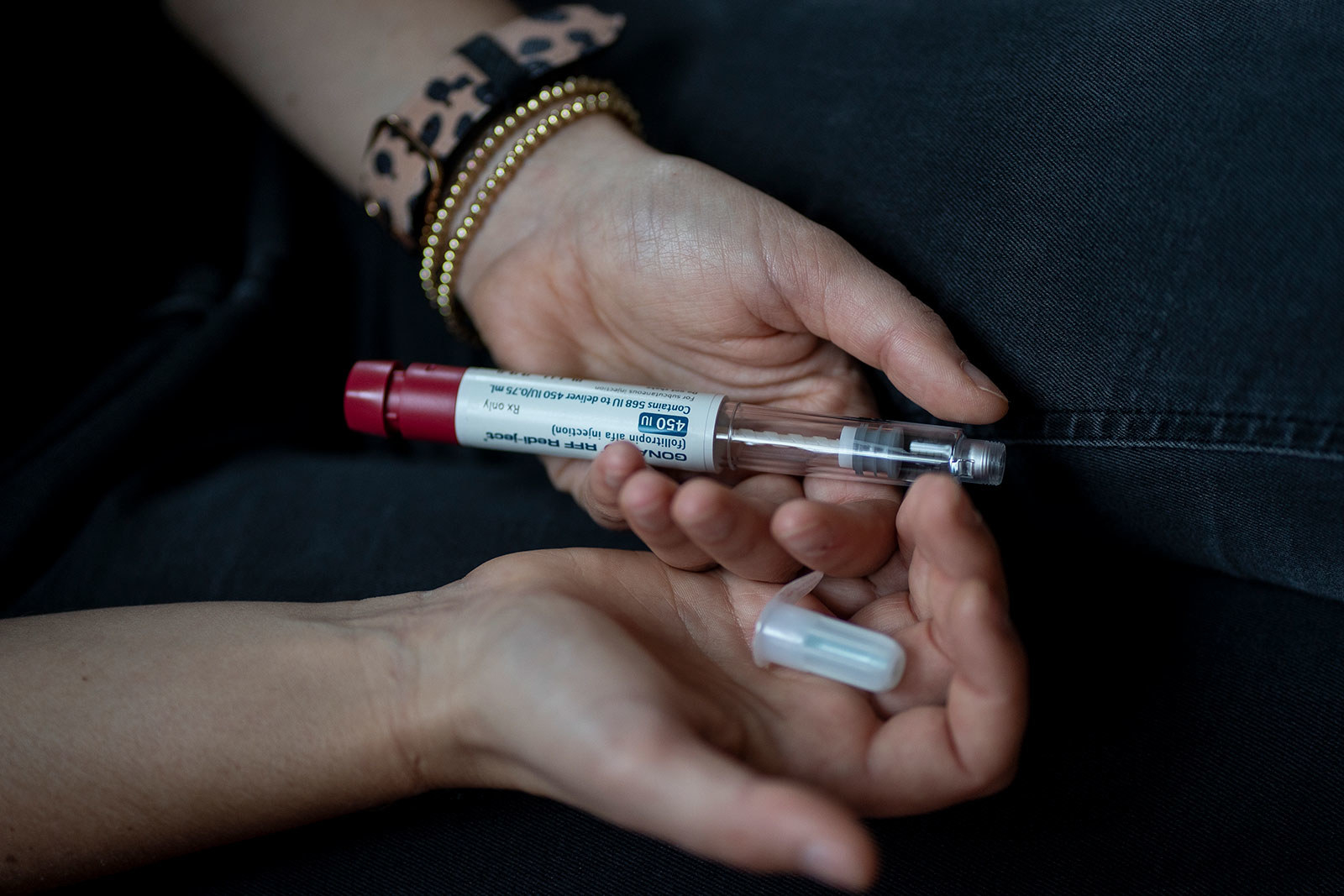
Though the process was over in two weeks, they were an intense two weeks. I injected myself with hormones twice then three times a day to stimulate my ovaries to produce several eggs. I had doctor appointments every other day, where they drew blood and conducted transvaginal ultrasounds each time. And while I had the emotional support of my partner through it all, I was still tired, stressed, and anxious. When my doctor felt that my follicles were ready for the egg retrieval procedure, I was brought into the surgery center 36 hours later and put into twilight sleep. The doctor used a needle with a suction device to retrieve my eggs. The procedure took less than 15 minutes. I came home and slept, and the next day, I couldn’t believe it was all suddenly over.
The experience, though short, was remarkably taxing on my body, alienating me emotionally, and — despite the fact that much of the process was covered due to anomalous infertility — financially burdensome. Once I got past the fear of injecting myself three times every day, there was still the question: Would these eggs turn into a viable pregnancy down the line if I wanted it? As research has shown, it was hardly a guarantee.
Decisions around childrearing impact people with uteruses in countless varied ways — and no story is quite the same. More and more people are seeking out the option to preserve fertility through egg freezing: A study published in the journal Fertility and Sterility in 2021 found a 39% increase in egg retrievals compared to prepandemic levels.
The choices people with uteruses have to make about their bodies are so rarely straightforward or neutral. Below, five people who have gone through the egg retrieval process describe what their experience was like, from the financial toll to the impact on their bodies.
The following interviews have been condensed and edited for clarity.
If I didn’t know that biology was not on my side, I would just carry on with my life the way that it is, because I absolutely love what I have. But I also want to be a mother. Last year, I was in a relationship, and I needed to have a plan B because I wasn’t looking to turn it into anything serious. So that’s when I thought, OK, let me do it.
COVID made me hyperfocused on life — the whole process of life and death. During that time, processing what was going on around me, I was just thinking, Well, what legacy do I want to leave behind? What do I want to achieve with my life, but also in the future? And I realized that I do wanna be a mother and that I wanted to be more serious and committed to that path.
But do I honestly, really, truthfully deep in my heart want to make an active choice to be a single parent? Because I’ve seen it and it is hard, and I do not want to step into something with a rose-colored, rose-tinted filter. You need community. You need a network around you. I certainly do have that, but there was a tweet that really made me laugh out loud, which was, “Everybody wants a baby until you are holding that baby at 3 a.m. and both of you are staring at each other crying.” There’s a reality check of what it takes. And it’s not about strength. It’s about that robust community that you have around. I want a partner in that. I want someone who is equally invested in having a family but also someone who is committed to me as to our child.
[When I decided to go through with the process], I spoke to a couple of friends who were going through IVF or freezing their eggs. I wanted to hear it from people who were doing it in real time. I didn’t defer to the internet because there can be an emotional detachment when you are reading information, especially when it pertains to this type of subject matter. I wanted to hear the theory about it, but I also wanted to hear [about] the emotional toll that it would take. Then I started looking around at different fertility clinics and then came the big ball buster: finding a clinic that accepted insurance. Then realizing, Oh, my health benefit doesn’t do shit.
[It] is so important that the clinic is as equally invested in your success as you are. The first clinic I went to, I never went back, because I felt like I was on a conveyor belt. I remember the doctor saying, “All right, we're gonna retrieve.” There were three eggs. And I said, “Well, shouldn’t we wait? That seems like such a low number.” No, we are gonna do it. So he did the retrieval and he got one [viable] egg. And I thought, I’ve just spent $14,000 on one egg. This one egg is my only chance to become a mother. The second clinic I went to? Phenomenal. I got eight eggs in two cycles.
I built it up in my head to be so much more than it turned out to be. I thought it would be this very long process of being at home and these needles and different things, but it’s six minutes of injections. That feels like a very short period of time for how much I paid. The way I look at it, though, is that the things that I am leaving behind or have left my life — in this case, the money — [are] making room for the abundance that's to come.
“I thought it would be this very long process of being at home and these needles and different things, but it’s six minutes of injections.”
In West Indian culture, there’s a tendency to be quite conservative around these matters. I had to bat, left, right, and center, “Where’s your man, where are your children?” I would try to get out of that by responding, “Oh, you wanna know about my sex life?” And as soon as you mention sex to an older West Indian, they back off. What was really nice is that I’m of that generation where we do openly talk about it and it is OK to not have a child. I feel that we are the first generation that’s really pushing that narrative forward.
People need to stop positioning somebody freezing their eggs [as being] because they’ve sacrificed something. “You focused on your job, you focused on traveling, you focused on your education and you sacrificed.” Why isn’t it that a woman was just living? We were just being.
*Name changed to protect privacy
In November of 2021, I found out that I had Hodgkin’s lymphoma, which is basically cancer of the lymph nodes. [Doctors] told me it was super treatable and the chemo shouldn’t affect my ovaries or any reproductive health, but they were like, “Just to be safe, we recommend [egg freezing].” I was referred to a specialist in LA.
You’d be shocked how busy these offices were at any time of the day that I went there — they were packed all the time, with different couples, people on their own. It’s pretty eye-opening to see how many women are doing this just to prevent issues in the future or just to have that backup. [The specialists] said you need to give yourself three shots a day and you need to take it easy, no strenuous activities. You can go on walks, but limit your carbohydrate intake and no alcohol. Obviously no drugs of any sort, no smoking. You really just need your body to chill out. For about two weeks, I would go in for blood work every other day and they would check my levels [with blood work], and they would check internally with an ultrasound to see how the egg follicles were forming. Basically, they want your eggs to be at a point where they’re ready to be retrieved. Then when the time comes, it’s kind of like, “All right, you’re having surgery today.” So it’s kind of a super fast process. They put you under, and it seemed like a pretty quick procedure.
A week after the retrieval, I had my first chemo treatment. You’re basically waiting for your period to come after the retrieval is done [and it tends to come with a lot of cramping]. When it came, it was the most excruciating thing. I don’t think I’ve ever had that much pain in my life. It’s kind of hard to say if it was the retrieval or the chemo that I was also going through at the time, but the chemo process was almost less bad than the physical pain of the cramping [when I got my period] — it just was unbearable. I don’t know if that’s the case for everyone or that was just me and my other circumstances going on, though.
They took out nine eggs and they were able to freeze five. I’m aiming to naturally get pregnant in the future. It’s good to know that I have that option and that those eggs are so many years younger than the eggs that I currently have.
My insurance covered a majority of it. I might have had to pay out of pocket for some of the hormones. Luckily, I had family helping me pay for the actual freezing part, which was I think $5,000 for the 10 years, and then it decreases per bracket [for subsequent time periods]. But overall, chemo was much more expensive than the retrieval. I’m in remission for my cancer now.
I wouldn’t say it’s a scary process. I think it’s definitely scarier when you need to do it versus just doing it preventatively. I think as long as you’re OK with needles and things like that, it’s just one of those things that you have to put in your day-to-day routine and just be good about all the other things that they recommend.
I was one of the first people in New York state who was able to get my part of the retrieval process covered with insurance because of my gender identity. I want other people in that position to know that that’s potentially a possibility.
I’m a teacher in the New York City public schools, so I have whatever insurance comes with that. I worked with a therapist for a while to get the documentation I needed to provide my insurance company. I was fighting with my insurance company for probably close to a year before a change in New York state policy provided genderqueer and trans people with coverage to be able to use their genetic material to reproduce. The note that I got from my therapist said that I was trans, and I think that language is maybe enough, but she included that it would be psychologically harmful for me if I were to carry.
My wife carried our first child, and for that we just did an at-home insemination. We knew that [this time], in an ideal world, she would carry my egg with the same sperm donor. So once it was possible for me to retrieve my eggs, we were able to do that. We worked with the fertility office, [and] the sperm donor that we used before was able to go and make a donation and they were able to make embryos — eventually my partner will carry.
We watched this show, Couples Therapy — there’s a trans woman on the show with a partner. I think they’ve since broken up, or maybe they broke up at the end of the season, but they went to a fertility doctor in Brooklyn and I was like, where did they go? It happened to be this doctor’s office down the street from where I live. It felt kind of magical. I felt like she really understood our family and my identity.

The actual egg retrieval was really hard. You have to go in three times the first week, and then I had to go almost every day the second week to do the blood work and ultrasounds and stuff. And then my mom was at my house when I was doing the first set of shots because we had a brand-new baby. I was really scared to give myself the shot, and I was watching the videos that they give you over and over again. I have polycystic ovary syndrome, and so my understanding was that they were gonna be really careful about how much medication I used, to try and keep it regulated. That’s not really what happened. I think they said it was [ovarian hyperstimulation syndrome], where many more eggs were growing than what they needed. When I went in to have the procedure done, they wound up taking out 26 eggs. A lot of them didn’t wind up being viable, but I looked the same as my wife at six months pregnant because my ovaries were so enlarged.
“I played rugby for 15 years. I’ve never been in pain like this.”
We went to do the egg retrieval procedure. You’re only there for a little bit, and they send you home with some painkillers. That night I remember lying in bed in so much pain that I couldn’t roll over or sit up. And my wife called the emergency line they had given us and the person on the phone was like, “Oh, it’s just totally normal. What you’re describing is completely normal.” I played rugby for 15 years. I’ve never been in pain like this. I think I eventually fell asleep, but the pain persisted for a few days and the swelling was so intense for so many days, close to a month after. I went back in and saw a different doctor who happened to be in the office and they told me again that it was normal for someone with PCOS. I wouldn’t wanna talk anyone out of this, but I didn’t know that that’s what it was gonna be like afterward.
I was fine with doing the ultrasounds and being in a space that was incredibly feminine in some ways, but I could imagine other people feeling much more uncomfortable in that kind of space and in that kind of environment. No one’s asking you your pronouns. I think for me the part that was the most uncomfortable was the way that I looked. I was physically uncomfortable and I was very aware of how I looked pregnant. I teach high schoolers and I felt like there were eyes on me in a different way. I have a lot of queer students and trans students here and I didn’t wanna have to deal with [explaining] while I was so physically uncomfortable.
I have actually been super private about my IVF stuff. A friend of mine started doing IVF and found out I had, and when I talked to her, I realized how much information wasn’t out there. So many questions that weren’t answered. I am married. I have been with my husband for 20 years and we have tried to conceive naturally for, oh man, we’re going on eight and a half years now. It came down to having really bad doctors that just didn’t listen and kept blaming it on everything else. And nobody ever took a simple test to check me. And I got a new OB who immediately did that test and was like, “Wait a second. Your chance of getting pregnant on your own is 1%.” So we did this fully with the intention of having a child.
The first thing that people should know going into this is it’s a very slow process. So it starts off with a lot of testing — even if they know, for me, that I have a low egg reserve, they still wanna do a litany of tests. I wanted to try to get pregnant. My first egg retrieval, I had 15 follicles. We got out of those 15 follicles 13 eggs. At that point, if I had wanted to just freeze the eggs and store them, that’s when they would store them. Then we fertilized those eggs — 10 of them fertilized. And then you have to wait one week for them to grow. And however many survive that growth phase, that’s how many embryos you have. For us, we ended up with five embryos, then we chose to do DNA testing and ended up with four embryos that you can transfer for the first round. The second round I had 22 follicles and they got 20 eggs. Four of them ended up surviving the growth phase and none of them were transferable. So we ended up with zero embryos from that one. It turned out that my embryos all came back with Turner syndrome, which is a chromosomal issue that is very high risk for miscarriage.
We did one transfer after our first egg retrieval. It was successful and we were really excited. Then, about 10 weeks in, I had my ultrasound and my fibroids had pushed my embryo into a position for miscarriage. I had a very brutal miscarriage and ended up having to do surgery to get the fibroids out because fibroids get really big when you get pregnant. The hormones just feed them and they knew that the risk of me miscarrying again is just due to the fibroids — my embryo was a perfect-grade embryo. I had surgery in August. You have to wait a period of time after surgery to make sure the uterus heals, and we’re hoping to do another transfer in July.

After I had my miscarriage, I bled for eight weeks. It was really tricky, because it was at the time when they overturned Roe v. Wade. There was a lot of stuff going on with the doctors trying to be careful because I live in Georgia, and of course we’ve got our Republican leaders here who were already making decisions. We had a trigger law in place that included not being able to get a medication called methylergonovine, which is commonly used in abortion, but it’s also used for other things. I already had these feelings of failure because my pregnancy didn’t work. I was actively losing my pregnancy. We had spent $20,000 on the first round of IVF. And I went to a doctor who told me, “your body cannot naturally pass this. What’s left of your pregnancy is currently stuck in your cervix and it can’t pass it. That’s why you’re continuing to bleed.” And he said, “I have to give you methylergonovine, which helps your uterus contract to push things out.” In the office, he was very concerned about me going into sepsis and he said, “I can get in there and I can pull this out, but I would need to do it right now.”
“I highly recommend anybody who does this has a very good therapist they can go to.”
He was not able to give me any numbing agents because I didn’t have anybody to drive me home — I thought I was just going in for a follow-up. The office was getting ready to close and Atlanta traffic is awful, so nobody could get to me. And he said, ”It’s gonna be very painful.” I’d been bleeding for eight weeks and I said, “Go ahead and just do it. I need this to be done before I get sick because right now with the way the laws are changing, they’re not gonna help me.” I laid on a bed while the nurse held my hand and it was the most painful thing I’ve ever experienced. He was so kind. He kept apologizing, but he was like, “We have to do this to keep you safe.” The emotional toll that takes is atrocious.
Coming up on the third egg retrieval, I had to do a lot of therapy. I highly recommend anybody who does this has a very good therapist they can go to. I told my husband and my therapist I didn’t know if I wanted to do it again because I felt like a science experiment. The doctors are poking your body all the time and everybody’s poking you and prodding you and testing you.
It’s really important for me at least with IVF to recognize the privilege we have that we’re able to even do it in the first place, because not everybody has the option of freezing eggs or freezing embryos. Even with that privilege, we have had to take out personal loans, loans from family members; we’ve had to charge credit cards. And then when you do that and it doesn’t work, there is a feeling of absolute failure.
Egg freezing had been on my radar for probably about two years or so. I had heard of other people in my network who had frozen their eggs, and so that put it on my radar as something I should think about. But I knew that it was a very expensive process, so I thought, Well, you know, I’m not at a point where I’m willing to spend that amount of money. I don’t really know anything about the process, but I’m not willing to spend $15 or $20,000 for this. Then I actually found out that my employer paid for it. I’ve been at my company for two and a half years, and I had no idea until recently that they paid for it. Because again, no one was really talking about that, and when they talked about our benefits, no one would ever say that. That’s when I started thinking, Huh, I’m 31 years old. I don’t see myself having children anytime soon. But I really want to be able to have that opportunity in the future, or I don’t know for sure if I want to have children in the future, but I wanna be able to have that choice in the future. And so it still obviously did cost me quite a bit because I do have — like a typical millennial — a high-deductible insurance plan.
I decided to go home to where my parents are located, in Buffalo, to do this process because I wasn’t really sure how it would be for my body. I wanted to be able to spend time at home relaxing and have my parents there when I needed someone to pick me up. I hadn’t realized that it was a multi-month process. I’d heard that the egg-freezing process is somewhere around two weeks, so I thought I’d go for a consultation early September, I’ll be done by the end of September. I had no idea people do multiple cycles, anything like that. That’s when [the doctors] started telling me it would be a three-month process if I was looking to just do one cycle, but a lot of people don’t get enough eggs in the first cycle, so it could take up to six months.
I am a health coach, so I knew the importance of keeping my stress levels low, of eating healthy, how much those sorts of things actually play into how the hormones affected me. I don’t have too much going on back in Buffalo, so I was truly outside of work, able to just relax and not have to worry about much, which was helpful on its own.
The actual procedure itself was no big deal. I went into the clinic and they gave me anesthesia and I don’t remember anything at all. Nothing hurt at all. The next thing I knew I was sitting back in a chair with my dad and they were talking to me about how it had gone. The problem was more that, six days after, I had terrible, terrible stabbing cramps. I had no idea it would be like that afterward. I know that doesn’t happen to everyone, but the aftermath was quite rough. On top of that, I didn’t get as many eggs as I wanted from the procedure, and I hadn’t realized how that would emotionally affect me. That was honestly very, very emotionally painful.
I find that most women my age have no idea about our fertility or the egg reserve that exists inside us to begin with. Many people are not getting it tested before they start considering egg freezing. So I found that really painful. I just assumed that it would be no problem, and I didn’t realize that my egg reserve going into this was lower and that that would be a challenge.
I’ve really considered whether I want to go through it again. After the retrieval, there was a lot of me that felt like, Why don’t you just let nature take its course now? I did what I did and it doesn’t mean I need to do it again. Because it’s pain on the body. It’s financial pain as well. On top of that, I know that adding extra hormones into your body is not a good idea. In the end, I just don’t see myself having children anytime soon. And to be honest, now that I’ve learned that my egg count is lower, it is really important to me that [I know this information now]. I am lucky where my job does pay for a lot of the process, and if I were to leave my job anytime soon, I don’t see myself being able to pay for [egg freezing]. ●
Dayna Evans is a freelance writer based in Philadelphia.





