Before childbirth, Sakinah Harrison had a great relationship with her body. “I loved the way I looked. I loved the way I felt. I was very confident,” she recalled. She worked out. She was mindful of what she cooked. Throughout her pregnancy, she remained active. But when she delivered her baby in 2019, he came quickly and suddenly. “In one go, his whole body came out of me,” she said. She ripped open. The doctor placed her baby on her body and told her in the dizzying moments after birth — while a person is meeting their child for the first time, while nurses are weighing and cleaning the baby, while you’re realizing that the pregnancy is done, you did it, and you are now a parent — that she had torn the tissue from her vagina to her rectum. “It didn’t resonate with me. … I was so zoomed in on my child and on myself that I really didn’t understand what was happening down below.”
When her epidural wore off, Harrison was in so much pain she started crying. “My vagina was so sore, and painful.” The doctor told her the tear would take 12 weeks to heal and the hospital released her three days after the birth. Just as her stitches healed, COVID shut everything down. People she knew died. Harrison got postpartum depression. In this time of isolation, “I started feeling something a little bit weird with my vagina,” she said “I ignored it, because I thought, I’m not going to the doctor. I’m not getting sick.”

When she felt it was safe to see a doctor in early 2021, Harrison was told she had stage 2 uterine prolapse, meaning the uterus had fallen into the lower part of the vagina. It can feel like pressure in the vagina, and it is visible. Lose the baby weight; do pelvic floor exercises, her doctor instructed. Harrison followed through — “I did it.”
One day, a year later, “I feel something rubbing on my inner thigh and I’m like, What is going on? I go upstairs — and I’ve been through a lot of soreness and things that are not normal down there — and I see meat coming out of my vagina, and I freak out,” Harrison said. She got an emergency appointment. Her prolapse had progressed to stage 3, meaning the cervix was now protruding from the vagina. “I'm like, No, no, no, no. I’ve lost the weight. I’ve done the exercises. I’ve done what you said. It can’t get worse.” But it did.
Several times a week now, Harrison, who also has endometriosis, has to push her uterus back into her body, and it has become retroverted, pointing backward instead of forward, causing back pain. She was fitted for two pessaries, a ring placed in the vagina to help support the pelvic organs, but they kept falling out. “It’s been a mental fight, because at this point, nothing’s working.” Her doctor said if she did nothing her prolapse could progress to stage 4, meaning the uterus falls outside the vagina. She could get a surgery to hold up her uterus, but the effects might be temporary, and getting pregnant again would be very risky, Harrison said. Now 37 years old, she is planning to have her uterus removed. She would not be able to carry children again, but she hopes it can improve her quality of life.
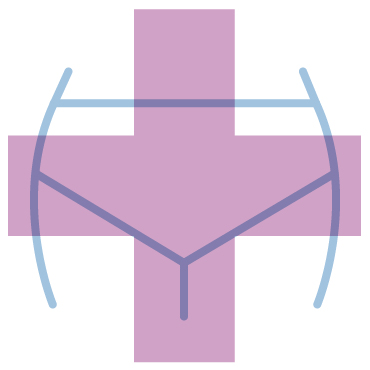
Pregnancy and childbirth have long-lasting impacts on a person’s body. While many people have simple recoveries don’t notice any changes to their vaginas and other pelvic organs (which include the cervix, uterus, bladder, urethra, and rectum), those who do may feel too embarrassed or ashamed to even talk to family and friends about it.
Pregnancy has the strange effect of being at once so public, a time in which the body is on display, and also deeply private. Some changes — stretch marks, deflated breasts, loose skin — are widely known and discussed. Celebrities and influencers share photos of these changes on their social media accounts in the name of body positivity, empowering people to embrace certain new features of their bodies. But no one shares pictures of their vaginas after birth. Postpartum recovery — mentally and physically — can be a lonely experience.
“I wasn’t informed about a lot of things I felt like I should have been told,” said Harrison, who is grappling with not being able to be pregnant again. “I feel I have let my husband down. I’ve let my son down; I cannot give him a sibling. … Having a uterus is all about feeling like a woman. That’s part of us — all the bleeding and all the craziness that comes with it, yes, it’s a lot, but it’s a part of me. And never in a million years would I have thought I’d have to give it up this early in life.”
I spoke with women around the country about the many ways the vagina and other pelvic organs can change after vaginal and C-section births. They told me about scar tissue from tearing in or around the vagina or from episiotomy (an incision made during birth) that can lead to tightness. (People can also have tightness after a C-section if the muscles become tense with hormone changes or postural changes.) Some had hormonal changes that caused dryness in the vagina that made sex uncomfortable or even painful. For others, sex positions that used to be pleasurable suddenly weren’t, making them feel out of touch with their bodies (although others said sex got better). Some felt their vaginas had endured trauma in childbirth, or were insecure about changes in the appearance of their vulva — such as the size of the labia, or new asymmetry, or seeing parts of their body that had fallen due to prolapse — and no longer thought of their genitals in the same way. Some can no longer wear tampons or menstrual cups because they slip out. Some suddenly found that their skin got irritated if they didn’t wear cotton underwear. Others queef much more than they used to. Some have incontinence and leak urine or feces when they exercise, cough, sneeze, or laugh.
The toll isn’t only physical, but mental as well. Over and over, women told me even though their OB-GYNs said they had healed by their six-week postpartum exams (this is typically when you are cleared to resume exercise and sex), they were now conscious of, and cautious about, their vaginas in a way they didn’t before childbirth. For some people, the changes led them not to trust their vaginas or their bodies anymore, and the lack of information and openness about it caused fear and shame. Even those who considered themselves informed about childbirth and recovery felt caught off guard.

“It’s not trusting your body, because it doesn’t feel like yours,” said Leigha Griswold, a 33-year-old who lost some bladder control after two pregnancies. She quickly returned to her prepregnancy weight (“It’s genetics,” she said), and “people would compliment me, but I was so frustrated with hearing that. I would scream in my head and want to say, ‘But my vagina is full of stitches,’ or ‘I’m wearing a pad because I pee myself now.’”
Griswold goes to physical therapy now to strengthen her core and pelvic floor to help with urinary issues. It’s been gradually getting better. “It’s a bit of a process.” She described it as “getting to know your body in a completely different way that you just didn’t have to think about before.”
One in three women experiences pelvic floor disorders while pelvic organ prolapse impacts about 1 in 4 women in their 40s in varying degrees and the rate increases with age, according to the American College of Obstetricians and Gynecologists. But research has shown that women of color are less likely to know about them and also less likely to receive treatment. Pelvic floor disorders “are highly prevalent in the primary care setting and should be screened for,” concluded researchers in a 2022 report.
One woman who has prolapse and asked only to be identified as A.R. said no one had ever told her about prolapse, not her midwife nor her close relative who works as a midwife. A.R. planned to have an unmedicated birth, but two weeks past her due date, her child was about 10 pounds and she had to be induced. Having prolapse now means A.R. feels a bulge in her vagina and has lost some bladder control; she wears a pessary. Sex is now less pleasurable, though she still enjoys it. Mostly, she feels more self-conscious about this part of her body. Although she is a former college athlete, CrossFit member, and runner, she suspects she’s had a weak pelvic floor her whole life, recalling that as a child she would leak a little urine if she was on her friend’s trampoline too long. It never got to a point where she felt the need to seek help until after her child was born. She wishes there had been a routine screening for such weakness before and during pregnancy. “If I had known the risks, I maybe would have induced earlier to have a smaller child,” she said.
Working out was once an outlet for A.R. to relieve stress, a pleasure, but now she is scared that many of the physical activities she enjoyed will make the prolapse worse to the point of requiring surgery (she goes biking and swimming instead now). “I spent a couple of months really, really depressed about the situation and the loss of identity as an athlete,” she said. A.R. has told few people in her own social circle about what she is going through, although she still wishes there was more information available about what to expect after birth. “It just feels like such a private part of my body,” she said. “I think the worry is that when people see me, they’ll always think of my sagging vagina.”
The lack of information and support (at home, at work, and socially) for people experiencing these changes makes it common to feel “broken” after childbirth, said Kristi Kliebert, a pelvic health physical therapist and spokesperson for the Academy of Pelvic Health Physical Therapy, a professional organization. “They feel like they've lost themselves. They feel like they don't know how they fit into the new norm.” The truth is some bodies return to something close to what they were like prepregnancy, and other bodies simply recover differently. Many conditions can be treated or improved. “The body is going to continue to change and it's going to continue to heal,” Kliebert said. “Everyone heals differently.”
Still, Kliebert said the fact that so many people are not well informed about how to care for muscles that are so critical to the health of people with vaginas, and lack access to treatment is indicative of “a systemic issue.” Primary care doctors and OBs may not do in-depth screenings for pelvic floor weakness before or after pregnancy, and health insurance may not cover physical therapy. It’s another layer to the challenges parents face in a country with no national paid parental leave policy.
The women I spoke with who sought help from pelvic floor therapy all strongly recommended it, even if they didn’t know what they were getting into. It’s an intimate form of therapy; you should find someone you feel extremely comfortable with. Depending on what you’re getting treated for, the therapist may also use their gloved fingers to assess the pelvic floor muscles, observe a Kegel or a cough, palpitate some areas, or do internal massage. There may be some core-strengthening exercises and help isolating and engaging the pelvic floor muscles.
Rachel Thennes, who works as an occupational therapist, was unable to hold her urine the entire time she ran in a 5K event after her son was born. “It was really embarrassing. Even knowing everything that I know about postpartum and pelvic floor, it was still like, ‘Oh my god, I can’t believe I’m peeing my pants in front of all these people,” she said. Sex also caused pain in the area where she had scar tissue from tearing; the lube her doctor recommended provided little relief.

Thennes decided to train in pelvic floor occupational therapy in 2020 and apply what she was learning in class to treat herself. “For class, you’re pretty much naked from the waist down the whole time. And it’s just a bunch of women standing around this room practicing on each other, which sounds super awkward, but you get over it real fast,” she said. “They taught us how to do perineal massage to help break up that scar tissue so sex wouldn’t hurt anymore. They explained that treating incontinence isn’t just doing Kegels — it’s about posture, breathing, body mechanics, behavior changes, and that your pelvic floor can be overly tight — not just loosey-goosey and need strengthening — and sometimes they’re so tight they need to learn to relax so that they can be functional. There were so many things that I would have never thought about, things that I didn’t even learn in my graduate program,” Thennes said. It changed not only the way she was caring for her own body, but also her career — she now specializes in the pelvic floor.
“I had a better understanding of what was going on, and it made me feel better that this isn’t just something that I go through,” Thennes said. “It’s something a lot of people go through, and I’m not just weird and bad.”
One of the most common injuries during birth is tearing — about 70% of people experience some tearing during birth. Often the tear is on the perineum, the tissue between the vaginal opening and anus, and it can range from a superficial tear of the skin (first degree) to a tear of both the skin and muscle (second degree) to a tearing of the anus (third degree) to tearing into the rectum (fourth degree). But there are other ways people tear that are less common and therefore less known. The clitoris and the tissue around it can tear, as can the labia, and vaginal wall.
Sierra Strassberg said at the end of 21 hours of labor, she had a periurethral tear, in which the tissue tears up toward the urethra. For months, the area was tender when she urinated. While she had heard about tearing of the perineum, “I didn’t know that you could tear at the top of your vagina,” she said. “I would have appreciated more information while I was pregnant.”
While Angela Betancourt did her best to reduce the risk of tearing — her mother was very open about vaginal birth and taught her about meditation to prepare for the delivery, and she also learned about perineal massage — she did develop prolapse. It made sex incredibly painful for her even though her doctor had cleared her for sex at her six-week exam with the recommendation to “use a lot of lubricant.” It was Betancourt’s mental health therapist who later told her it would take a lot more than lube to find her way back to intimacy.
With the pressures of caring for a baby, she said it now takes more effort than before to get in the mood for sex, including feeling taken care of on a daily basis by her husband, and loved and supported by him in small ways — feedback he has been receptive to. “The more that I leaned into getting my libido back, the less the other issues got in the way,” she said. “There was definitely some prolapse going on but […] it was very much a mental thing as well as physical.”
For so many women, being at peace with your body is a constant struggle. My interviews suggested that even people who tried their best to prepare, who were physically active, who did Kegel exercises and perineal massages were not all able to control what happened to their bodies after birth. I asked the women why they wanted to share their stories, despite their complicated emotions about changes they were going through privately. For the most part, they said they just wished someone had told them what might happen to their bodies — to their vaginas — after childbirth. It might have made it less scary and lonely; they might have felt less defective, less at fault, if they knew other people were going through similar things too.
Sakinah Harrison feels it is unfair that she was forced to decide whether to remove her uterus, but she recently started sharing her story within her inner circle both for her own sake, and to help them be “stronger and wiser.” “I can’t keep this in anymore. It’s now part of my life,” she said. She has appreciated the calls checking in, the meals people bring her, and their company.
“I’m not going to continue to hide natural things are happening to women. It’s all natural. It might not be the norm to you, but it’s actually the norm for a lot of women out here who’ve experienced what I’ve experienced,” Harrison said. “Women need each other. We feel alone in so much, and we try to take on so much. But we give birth. We give life. And it comes with a lot.” ●