First, the good news. Fewer young people — aka those in their thirties, forties, or early fifties — are getting lung cancer than in the past, regardless of race or gender.
Why? Because fewer people are smoking, which is good. (But as an aside, more than 25% of all cancer deaths in the US are still caused by smoking, so try to quit, y'all.)
Because men in past generations were more likely than women to be cigarette smokers, men have always had higher lung cancer rates than women. But that's no longer true: Women ages 30 to 49 are now more likely to get lung cancer than men, according to a report published today in the New England Journal of Medicine.
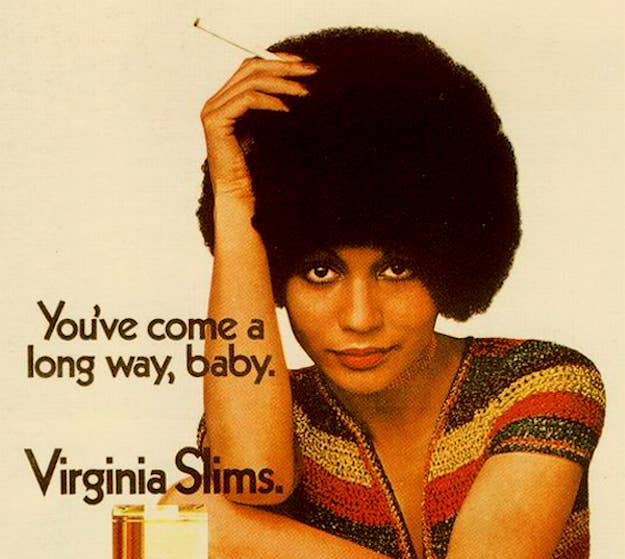
Given that cigarette manufacturers heavily marketed cigarette brands to women starting in the 1970s, the finding is not that surprising. The first cigarette designed specifically for women, Virginia Slims, was launched in 1968 with the slogan "You've come a long way, baby" and aimed to link cigarette smoking with the women's liberation movement. And indeed, smoking behavior changed over time and more women took up the habit, although they are still slightly less likely to smoke than men.
Smoking rates in women and girls went up "dramatically" in the 1990s due to tobacco company marketing, before eventually declining, according to the Campaign for Tobacco-Free Kids, and about 13% of adult women and 6% of girls in high school smoke.
"You've Come a Long Way Baby, for Virginia Slims by Philip Morris, definitely contributed to this," lead study author Ahmedin Jemal told BuzzFeed News. Jemal is the scientific vice president of the Surveillance and Health Services Research program at the American Cancer Society, which published the study with the National Cancer Institute.
Between 1995 and 1999 the lung cancer incidence — the number of cases per 100,000 women per year — was 26% lower in women ages 44 to 49 than men the same age. But between 2010 and 2014, the lung cancer incidence was 8% higher in those women.
The higher lung cancer rate in women than men was true for non-Hispanic white and Hispanic women. While lung cancer rates aren't yet higher in female non-Hispanic blacks and Asians/Pacific Islanders in the US, they are getting closer to crossing over, Jemal said.
However, more smoking doesn't entirely explain the higher lung cancer rates in women.
Because women are still slightly less likely to smoke than their male counterparts, the researchers think there might be some other factor that is playing a role. "We have three hypotheses of what may have contributed to this," Jemal said.
Some research suggests that once they start, women may be less likely to quit smoking than men. And although lung cancer (and other risks) tend to plummet once you quit smoking, the risk for one type — adenocarcinoma — takes a bit longer to go down. Women are more prone to this type of cancer than men, said Jemal.
In general, lung cancer risk drops 25% in the first five years after quitting, 50% after a decade, and 90% after 20+ years of not smoking, Jemal said.
It's also possible that women are more susceptible to the negative health effects of smoking, which have gotten worse over time, Jemal said. The advent of "light" cigarettes caused people's smoking behavior to change in a way that actually increased the cancer risk, he said.
"The puff volume is larger and the frequency of puff has increased, so the relative risk of lung cancer from smoking has now reached 25 times higher compared to nonsmokers," Jemal said. Two to three decades ago the risk of cancer was tenfold higher in smokers versus nonsmokers, he said.
About 10% of men and 15% of women with lung cancer have never smoked, so it's also possible that some women are more susceptible to non-smoking-related lung cancer, Jemal said, although that has not been proven.
Regardless, the message is still to quit smoking, and the younger the better. People who quit at 30 might get an average of 10 additional years of life, while quitters at 50 gain five years, and people in their sixties who quit gain three or four years, on average, Jemal said.
"Quitting at any age is beneficial, but it’s best if you quit at younger ages," he said. "Smokers have to seek quitting services — you have to ask for counseling and treatment."
