
Less than three weeks out from an election that many see as a referendum on President Donald Trump’s handling of the coronavirus pandemic, a “third wave” of COVID-19 hospitalizations is underway in the US.
Coronavirus cases and hospitalizations are now rising again across most of the nation, including the Northeast. But some of the biggest surges are currently happening across the Midwest and the northern plains, including Montana, Nebraska, and the Dakotas — states that escaped the worst of the previous two big surges in the spring and summer.
COVID-19 cases and hospitalizations are rising across the US
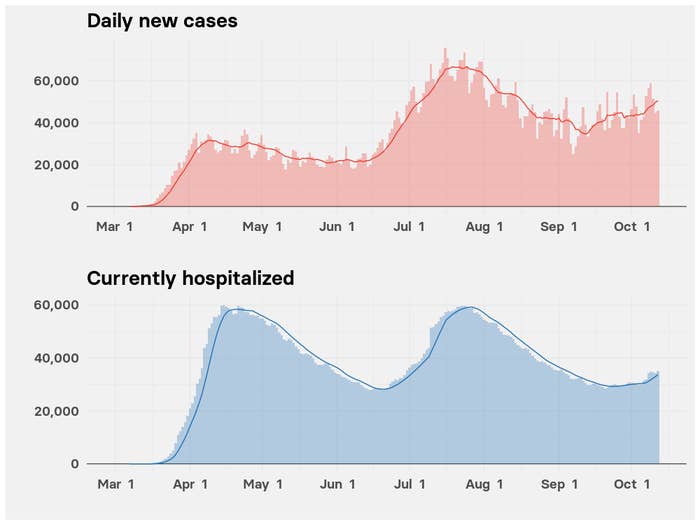
The plot of new confirmed cases shows three surges. Strictly speaking, these aren’t distinct waves of infection, like those seen in Western Europe. In those countries, cases surged in the spring before dying down and are now surging for a second time — triggering new lockdowns, including a nighttime curfew in Paris and eight other cities, announced today by French President Emmanuel Macron.
But the US never brought transmission of the virus back to a low level, allowing hot spots of infection to move around the country since March in what some have called a “patchwork pandemic.”
Hospitalizations for COVID-19 show up in the data later than case counts, and it’s unclear whether the current surge will rise as high as those in April and July. Those surges hit hardest in the Northeast and the Sun Belt, respectively, and each peaked with around 60,000 people in the hospital across the US.
The initial surge, centered on New York City and the surrounding area, plus Detroit and New Orleans, was much more deadly. Hospitals got completely overwhelmed. Doctors also then didn’t know how best to treat COVID-19 patients, lacking drugs, such as the steroid dexamethasone and the antiviral remdesivir, that are now used to treat those who are most severely ill.
But clinicians on the front line are concerned that another big rise may be on the way. “Clearly there are clouds on the horizon, and there are some very worrisome trends,” Mark Rupp, chief of the Division of Infectious Diseases at the University of Nebraska Medical Center in Omaha, told BuzzFeed News.
The current wave in hospitalizations, which began in September, hit especially hard in Wisconsin. Almost 1,000 people are currently hospitalized with COVID-19 in the state in a surge that shows no sign of slowing, according to data compiled by the COVID Tracking Project. About one-quarter of those patients are in the ICU.
On Wednesday, the state opened a field hospital that can house an additional 530 coronavirus patients, constructed in the Wisconsin State Fair Park outside Milwaukee to ease the pressure on the state’s regular hospitals. It is intended to treat those already on the road to recovery.
Worryingly, states to the west across the northern plains are following a similar trend.
People hospitalized with COVID-19 in four states across the Plains
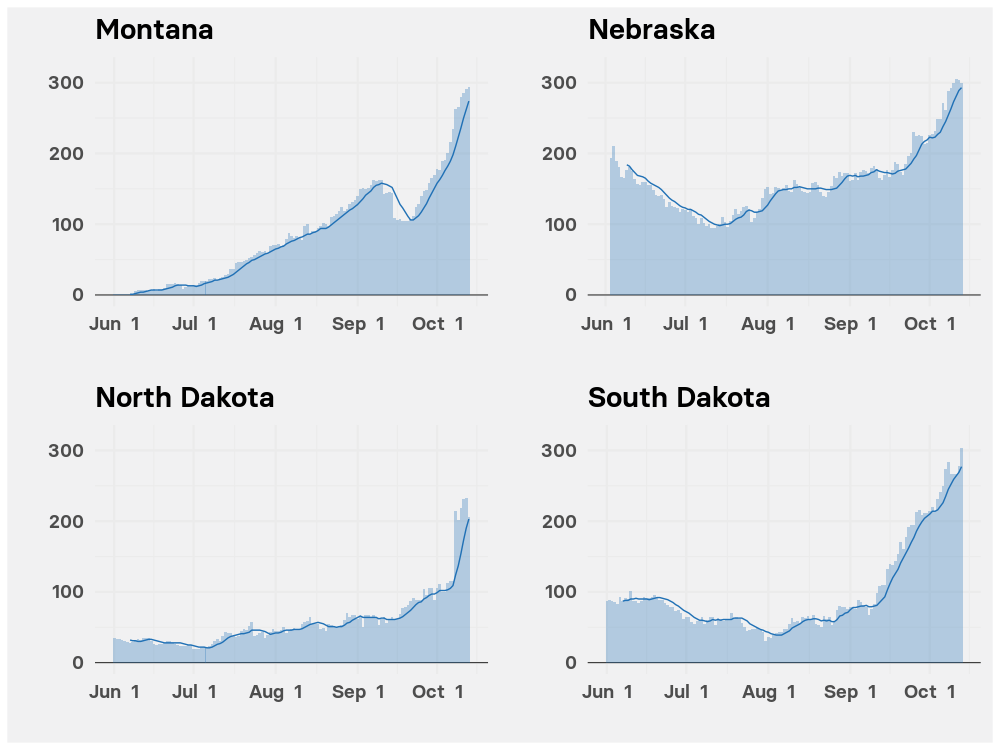
For the sparsely populated states of Montana and the Dakotas, this is the first major surge in COVID-19 hospitalizations.
Hospitals in North Dakota are nearing capacity, Renae Moch, public health director for Bismarck, the state’s capital city, told BuzzFeed News. Right now, she said, there was just one free ICU bed across the city’s two hospitals.
While it is possible to convert other beds to treat COVID-19 patients, capacity can’t be expanded indefinitely without affecting the quality of care, Moch said. “Would you want your family member set up on a cot in a field hospital?” she asked. “We have to make some sort of a change to prevent that from happening.”
Nebraska experienced a previous smaller surge that peaked around Memorial Day. During that time, the burden fell on leading medical centers, which took patients from around the state, Rupp said. His center was then forced to cancel elective procedures and clinic visits.
“We could do that again if absolutely necessary,” Rupp said. But, given the secondary health impacts on non–COVID-19 patients, it’s a step hospital administrators want to avoid.
In the current surge, local hospitals are taking more of the strain. But still, the University of Nebraska Medical Center is running at close to full capacity, Rupp said.
For Rupp, the biggest frustration is that the current surge could have been avoided if Nebraska hadn’t almost completely relaxed its COVID-19 restrictions. The state is currently in phase 4 of its reopening plan, with outdoor venues able to operate normally, indoor venues at 75% capacity, and gatherings of fewer than 500 people allowed without special permission from health officials.
Rupp said he understands why people feel fatigued with COVID-19 and want to get back to their normal lives — but that is putting a big strain on doctors, nurses, and other medical staffers.
“There’s nobody more COVID-fatigued than the people who are taking care of these patients,” he said.
Stephanie M. Lee contributed reporting for this story.
