In the wake of the Germanwings tragedy, mental health advocates are deeply concerned about misleading generalizations that may increase the stigma surrounding depression and make people less likely to seek the help that they need. But there's been little discussion of perhaps the most misleading generalization of all: the label "depression" itself.
What we call depression seems to be a grab bag of conditions involving different parts of the brain's circuitry. And while it's still early days, a fresh understanding of depression's diversity should lead to better treatments.
About 7% of U.S. adults experience at least one episode of major depression each year, according to the National Institute of Mental Health (NIMH). In terms of how many healthy years it takes from people's lives, depression is the most damaging of all the mental and behavioral disorders. Yet according to the latest research, major depression isn't a distinct disorder after all — despite being listed as such in the psychiatrists' bible, the Diagnostic and Statistical Manual of Mental Disorders.
"When we throw around the label 'depression,' we can often be referring to very different things," Daniel Foti, a clinical psychologist at Purdue University in Indiana, told BuzzFeed News.
Some of the confusion arises from the fact that depression is in many cases a secondary symptom of another mental disorder — about three quarters of people who meet the DSM's criteria for major depression have at least one other psychiatric condition. But even "pure" cases of major depression can manifest themselves very differently: Some people lose interest in activities they once found pleasurable, while others become unusually sensitive to negative experiences. Still others become irritable and angry.
Little wonder, then, that doctors struggle to diagnose the condition. Before the last rewrite of the DSM in 2013, the American Psychiatric Association ran trials in which different clinicians were asked to diagnose the same patients turning up at academic psychiatric hospitals. Major depressive disorder was among the hardest diagnoses on which to get agreement, getting a rating of "questionable" reliability.
For scientists trying to understand depression and develop new treatments, that was a wake-up call. "The problem is it's not one thing," NIMH Director Thomas Insel told BuzzFeed News. "That's why you have these low levels of reliability."
But psychiatric research is going through a shake-up.
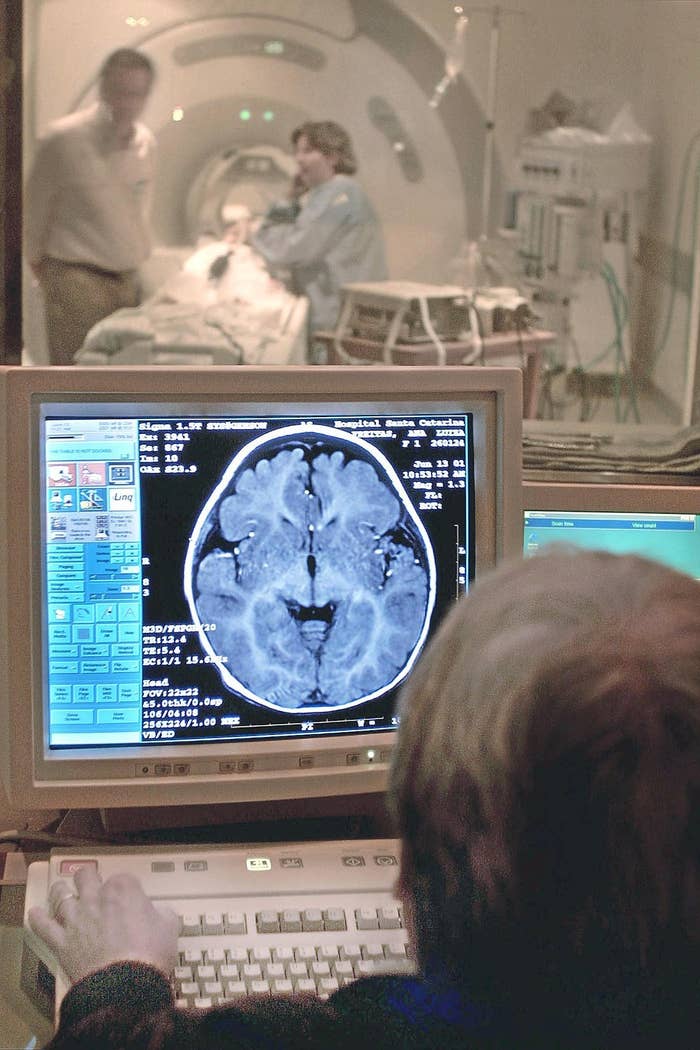
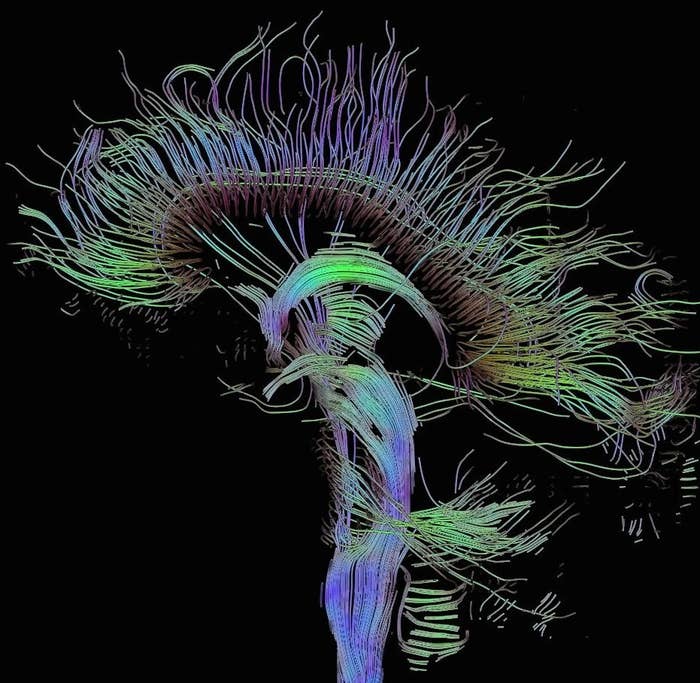
In April 2013, Insel announced that the NIMH would shift its $1.4 billion annual research budget away from projects focusing on DSM diagnoses to instead concentrate on underlying disturbances of brain circuitry. That means using brain imaging to look at the activity of these circuits, as well as studies of brain chemistry, genetics, and thinking patterns. It will also mean studying people with conditions that cut across the disorders defined by the DSM's checklists of symptoms.
In a blog post, Insel highlighted depression in explaining how things would change: "Clinical trials might study all patients in a mood clinic rather than those meeting strict major depressive disorder criteria."
The new approach is starting to bear fruit, as scientists make distinctions between different forms of depression. One type, for example, involves the brain's reward circuits. Another seems to be linked to impaired communication between the front of the brain and the amygdala, an area deep in the brain that processes emotions. The first type seems to be responsible for a phenomenon called "anhedonia" — an inability to feel pleasure — while the latter may help explain why some people are likely to be pushed into depressive episodes by negative life experiences.
Anhedonia may be particularly important, as people who don't feel pleasure also tend to respond poorly to psychotherapy and antidepressant drugs, and are more likely to have thoughts of suicide. "Even after you control for other depressive symptoms, it's a contributor to poor outcomes," Diego Pizzagalli, who heads the Center for Depression, Anxiety and Stress Research at McLean Hospital in Belmont, Massachusetts, told BuzzFeed News.
Up to half of people with depression fail to respond to treatment with an antidepressant. One big hope is an anesthetic called ketamine: It seems to alleviate anhedonia, and brain imaging indicates that this improvement is linked to increased activity in parts of the brain known to be associated with anticipating rewards. The drug also reduces suicidal thoughts, and is fast-acting — on the order of hours and days, rather than weeks.
Ketamine will probably not itself be the next blockbuster antidepressant. Also known as "Special K," it has hallucinogenic effects and is often used as a recreational drug. But after a period in which companies backed away from developing new antidepressants, big pharma is now developing drugs that mimic ketamine's influence on depression without causing hallucinations. AstraZeneca, for instance, is working on a ketamine mimic called lanicemine.
Some psychiatrists say it's too early to subdivide depression into different disorders.
Despite the difficulty defining exactly what it is, the label depression provides "a useful shorthand" for doctors to talk to their patients, Simon Wessely of King's College London and president of the Royal College of Psychiatrists, told BuzzFeed News.
Wessely said he is worried that patients may be put into new pigeonholes that are no more valid than the old DSM labels — which is unlikely to lead to better treatments. "We might end up making the wrong splits," he said.
Insel has also gotten some pushback from mental health professionals who fear that the new focus on brain circuitry will lead to an over-reliance on using drugs at the expense of other approaches to therapy.
But Insel disagrees that this will happen. "It's been a misunderstanding for many people," Insel said. "If we can begin to define these as brain circuit disorders, then treatments will become ways of tuning those circuits."
That tuning might involve drugs, but could also come from psychotherapy, or computer games aimed at changing specific behaviors or emotions.
