
The journalists at BuzzFeed News are proud to bring you trustworthy and relevant reporting about the coronavirus. To help keep this news free, become a member and sign up for our newsletter, Outbreak Today.
With COVID-19 raging through nursing homes in every corner of the nation, the US government last month suspended routine inspections, a critical layer of oversight designed to protect elderly residents from dangerous conditions.
A new BuzzFeed News analysis casts into sharp relief the hazards of the decision, which comes as thousands of nursing home residents are dying and family members are not allowed to visit. Facilities are now allowed to perform their own inspections, but the troubled track records at many homes suggest this will put vulnerable and isolated residents at even greater risk.
In the last two rounds of inspections, about 60% of nursing homes were cited for failures in infection control, the analysis found. Such breaches can lead to a host of ailments, including the flu, pneumonia, skin diseases — and the coronavirus.
Inspectors found caretakers hadn’t isolated residents during influenza outbreaks, didn't clean medical equipment, and didn't wear protective masks and gloves when treating vulnerable patients.
Regular inspections also turned up residents suffering from gaping, infected wounds; nurses giving the wrong prescriptions; and residents left alone with no one on duty. More than 7 out of 10 homes were operating with staffing levels below federal recommendations, an issue that is one of the leading causes of abuse and neglect in these kinds of facilities.
The Centers for Medicare and Medicaid Services announced last month it was temporarily halting regular inspections to more than 15,300 facilities so the agency and the facilities can focus on the imminent threat posed by the novel coronavirus. It’s a radical shift, coming at precisely the moment so many families and residents are left to communicate only by cellphones and laptops — or not at all.
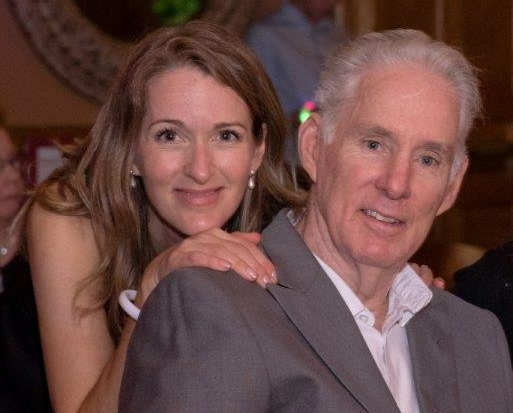
For Krista Hennessy, whose 79-year-old father died of the virus in a New Jersey facility, the inspections offered a crucial safety net for the people he left behind. “With the state not watching, it's only going to get worse,” she said.
The CMS said it will conduct targeted surveys of homes fighting the virus, looking for infection control threats, and respond to residents in immediate danger. States, which share in oversight with the federal government, will follow suit.
That decision already has led to a drastic reduction in oversight, records show.
If you're someone who is seeing the impact of the coronavirus firsthand, we’d like to hear from you. Reach out to us via one of our tip line channels.
To carry out their new mission, inspectors visited 96 homes from March 23 through April 10 and found that nearly 1 in 5 were not properly using protective equipment such as gloves or masks. During a similar time frame last year, inspectors carried out 925 routine surveys and turned up more than 6,000 violations for a range of problems, including bedsores, wrong prescriptions, and patients with cognitive impairments wandering out of facilities.
The agency didn’t respond to questions from BuzzFeed News about the risks of canceling the routine visits, nor did it say when the new policy would end.
But in a memo to state inspectors last month, it noted the shift "will allow health care providers time to implement the most recent infection control guidance from both CMS and the Centers for Disease Control and Prevention.”
Elder advocates, however, say the change in procedure creates a new level of danger, especially in those centers that have been plagued for years by abuse and neglect.
"It's going to result in horrific cases," said Brian Lee, former chief long-term care ombudsman for Florida's Department of Elder Affairs. "If there was ever a time to promote more oversight, this is the day and age when we need it."
The combination of aging residents, inadequate staffing, and the inability of caretakers to treat the rush of sick patients has created environments for the virus to take a dramatic toll on long-term care homes.
Despite the hardships inside the facilities, the federal government has not tracked which homes have the coronavirus, but recently announced that it will start. Several news organizations have collected data from the states, including the New York Times, which last week reported 3,800 long-term care centers with cases and at least 6,900 deaths, including residents, staff, and others tied to the homes.
The American Health Care Association, a trade group for nursing homes, defended the government's decision to lift the inspections, saying they would take time away from the front-line work. “Now is not the time to see if policy and procedures are up to date,” the group said.
However, Cyndy Minnery, a California health care expert who once did surveys for an Indiana nursing home chain, said routine inspections are critical to detecting hazards and, ultimately, saving lives.
"I just feel bad for the people who are still in there. They need to be protected."
"I'm talking about the homes with chronic problems," said Minnery, who advises law enforcement agencies on elder abuse cases. "There's got to be oversight. You walk the halls and you watch the staff. That’s where you’re going to see the breakdowns."
And Lee, who now runs Families for Better Care, a nonprofit for residents and their families, said that in his experience he’s encountered homes beleaguered by a host of severe problems: slipshod medical care, neglect, and decrepit conditions.
For example, records examined by BuzzFeed News show that in more than 3,300 homes since 2018, inspectors found patients with pressure sores — some so large and gaping that the flesh was rotted and the bone exposed. Records also show that more than 1,200 homes were cited in that same period for medication errors, including caretakers dispensing the wrong prescriptions and, in some cases, not giving patients their drugs at all.
At Maryland's Pleasant View Nursing Home, where 121 staff and residents have been infected and 26 died, inspectors previously found a host of deficiencies, including unsatisfactory infection control, a lack of critical care plans to address residents’ medical problems, and a failure to keep accurate medical records. In a rating system from one to five stars, the home was given the lowest by CMS.
Rob Holmberg, whose father, retired Washington, DC Fire Department Capt. Gary Holmberg, died with the virus on March 29, said he grew angrier as he read the inspection reports.
"I just don't know how they could have stayed open," he said.
He and his sister, Tracy Shavell, have formed a support group for relatives whose loved ones and residents who are still inside.
Shavell said the facility, whose staff was briefly augmented by the National Guard, needs full inspections.
"They can go in there with hazmat suits," she said. "I just feel bad for the people who are still in there. They need to be protected."
A spokesperson for Pleasant View said the facility declined to comment.
In the New Jersey facility where Krista Hennessy’s father lived, coronavirus wasn’t the first deadly illness to hit.
Just two years ago, a virus swept through and killed 11 children, leading to a scathing state report that cited the home for failing to respond to the sickness in a timely manner and provide adequate care.
During an unannounced visit to the home, which cares for people of varying ages, inspectors found staff members not washing their hands properly, including one who changed a soiled diaper while wearing gloves and then, without removing them, grabbed a respiratory tube and inserted it into a patient’s breathing device.
Then known as the Wanaque Center for Nursing and Rehabilitation, the facility later was sold and renamed the Phoenix Center for Rehabilitation and Pediatrics.
When the coronavirus struck, Hennessy and her family knew her father, Art Olsen, might be at risk, especially when his roommate tested positive. They asked to have him transferred to another room but were told, Hennessy said, he would first have to wait for his own test results.
After several days, the tests came back positive. Four days later, he died.
“It's almost like when they see someone in my dad's condition, in my opinion, they kind of give up,” she said. “They don't see any reason to keep them alive.”
The facility did not answer questions from BuzzFeed News about Art Olsen. In a written statement, a spokesperson said that it was following the guidance of federal and state health officials "and our infectious disease doctors while caring for our residents who are positive or suspected of having COVID-19.”
Lee, director of Families for Better Care, said the impact of not carrying out inspections depends on the duration but could be felt for months and years to come if facilities continue to run without any oversight.
In the meantime, the federal government has asked nursing homes to carry out their own reviews through a self-guided checklist, a CMS spokesperson said. The agency does not collect the assessments but can review them during later visits.
Florida attorney Bill Dean, a former Miami-Dade prosecutor who represents families in nursing home death cases, said he's leery of letting any facility — especially one with a troubled record — regulate itself.
“With no inspections, are we supposed to expect that they are going to do the right thing?” he said. "It's a sad situation that we've come to this in our country, that now we are at a point that we are going to let the nursing homes self-regulate.”

