
Yes, you can have two vaginas. Just ask Scarlett Rose, who didn’t find out about hers until she was 21 years old and 21 weeks pregnant.
Rose never had a reason to question (or count?) the anatomical features of her reproductive tract until she became sexually active in her late teens. Every attempt at penetration brought her excruciating pain. Tampons were absolutely off the table. Still, everything looked and felt “normal” down there, the 30-year-old from Australia recalled in a TikTok video that has been viewed nearly 10 million times.
Chalking it up to nerves, Rose would try to have sex again. And again. And again — to no avail. The pain was too intense to bear, so she temporarily called off relations with men altogether, assuming she wasn’t ready for intercourse.
In the meantime, she spent years visiting different doctors and undergoing tests so painful she would bleed, only to be misdiagnosed time and time again.
First, doctors told her the painful sex was due to stress and anxiety. Then they thought she might have polycystic ovary syndrome, a hormonal disorder that makes ovaries swell and sometimes develop cysts. After that, it was vaginismus: a condition caused by involuntary spasms or tensing of the vaginal muscles due to fear of penetration or prior injury to the area.
“I was following every treatment plan doctors advised, even with awful side effects from some of the treatments, and when they weren’t successful I blamed myself,” Rose told BuzzFeed News via email. “When they’d told me it was all in my head I just felt even more embarrassed and it left me feeling very broken.”
It wasn’t until Rose was pregnant and had to have a procedure to address her short cervix — a condition that increases the risk of preterm labor or premature birth — that she learned what was wrong.
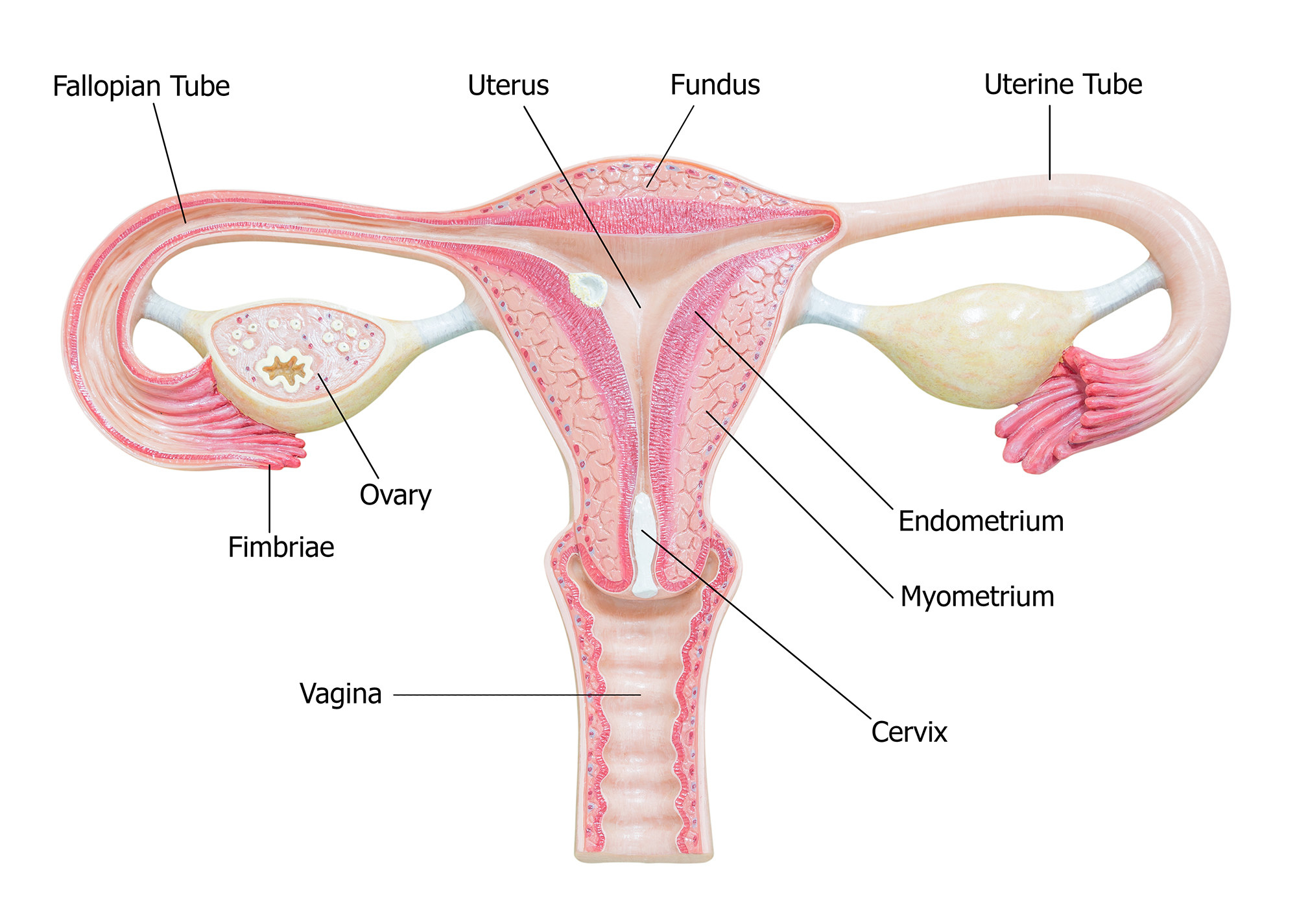
A band of flesh called a septum, which she’s had since birth, was separating her vagina into two sections. Every time doctors would examine Rose’s pelvis, the tools they used would push the septum to the side and successfully reach her cervix, appearing as if everything was normal. However, any painful shove would tear the septum, explaining why she bled after some exams. The septum also didn’t extend to the opening of her vagina, so it wasn’t obvious during exams.
Rose’s doctor removed the septum during the procedure on her cervix, thus turning two vaginas into one and finally giving her the freedom to enjoy pain-free sex.
“It all functions normally. I don’t have any pain at all during intercourse anymore, but [my doctor] did say that I was so lucky … because had I tried to deliver our baby naturally with that septum in place with two vaginas, I would have bled to death,” Rose says in a TikTok. “I just wanted to share this because it is very, very rare, but I … thought maybe it might help somebody out there who's struggling with pain and their doctor can't find the issue.”
Rose was moved when she read dozens of comments from women who said that they have the same issue and experienced similar problems getting an accurate diagnosis.
Her story shines a light on the difficulties people face in understanding and treating pelvic pain.
“There’s lots of different organs in our pelvis — the bladder, female reproductive system, bowels, rectum — so when we’re having pelvic pain, sometimes it’s just really hard to figure out what’s causing it,” said Dr. Allison Rodgers, an OB-GYN and reproductive endocrinologist at Fertility Centers of Illinois. “It's very uncommon for you to be able to do an ultrasound and find the cause of your pain and have a doctor say, ‘Let me give you this magic pill or do surgery and then you're fixed.’”
Not to mention, Rose’s condition is “notoriously difficult to diagnose because regular ultrasounds may not pick it up,” Rodgers said, adding that it requires different kinds of MRIs and/or ultrasounds “and somebody reading it who knows what they’re doing.”
Any malformation in the female reproductive system, including the uterus, cervix, fallopian tubes, and upper part of the vagina, is called a Müllerian anomaly. Up to 7% of the general population has at least one.
These anomalies occur around six weeks after conception, when the tubes that are supposed to mature into reproductive organs don’t develop properly. The glitch can leave some people with two cervixes, two uteruses, or two vaginas (or a combination of these options); others may be born with one of these organs missing or organs that develop into abnormal shapes and sizes.
In fact, about 90% of Rodgers’s patients are diagnosed with a different Müllerian anomaly than they actually have: “This is a very niche area and I think if they’re not doing this all the time, some doctors may not really understand the differences between all of these anomalies,” she said. “Even really smart, really educated doctors a lot of times will get this wrong.”
Vaginal septums, specifically, occur in about 1 in every 5,000 infants, so “it’s uncommon, but it’s also not rare,” Rodgers said.
Most people don’t notice the fact that their vagina is separated in two until they try to insert a tampon, have sex for the first time, or undergo several pelvic exams due to infertility or menstruation issues.
And a lot of the time, people with two vaginas won’t ever experience any issues with them, Rodgers said. Sometimes sexual partners may have to penetrate at certain angles or simply “choose a side,” while some people have to use two tampons during their period. One person commented on one of Rose’s TikToks that they birthed a child “out of each side.”
Vaginal septums can be painful and dangerous, however. Transverse septums, for example, form horizontally in the vagina and can partially or completely block menstrual blood from flowing out, which can cause abdominal pain. Other types may interfere with fertility. In these cases, septums may need to be surgically removed.
Some people with Müllerian anomalies could also be born with one kidney because the organs develop close to the reproductive system in the womb.
If you’re dealing with pelvic pain, Rodgers recommends addressing your concerns with a gynecologist, preferably one specialized in reproductive endocrinology, and being open to doing a series of exams and trying some medications to see what works and what doesn’t.
Most importantly, she urges you to advocate for yourself in the event you’re not getting any answers or your doctor isn’t taking you seriously.
Rose agrees.
“A lot of women deal with pain during sex and are too embarrassed to talk about it with anyone. I felt extremely alone when I was going through this and I didn’t want anyone else to feel like that,” said Rose, who created a podcast called Resilience in response to the feedback she got from her TikTok videos.
“It’s so common that women’s issues are dismissed or ignored and it’s just not acceptable,” Rose told BuzzFeed News. “Knowledge is power, and you can get so much further with doctors when you go into an appointment equipped with at least some idea of what might be going on, rather than going in blind and just having to accept whatever answers the doctor gives you.”
