In a random 24-hour period this week dozens of women have described their nausea, breast tenderness, anxiety, hurting joints, fatigue, inability to exercise, sore neck, weight gain, depression, infertility, mood swings, bleeding and psoriasis which they are convinced is the fault of their hormonal intrauterine devices (IUD).
This is not an unusual level of activity in the many private Facebook groups where thousands of Australian women gather every day to share stories and advice about their IUDs.
A few weeks earlier one woman asked whether she should remove the device from her cervix herself and was assured by others in the group it was fine as long as she kept her hands and fingernails clean.
A quick search revealed many in the group claimed they had ripped out their IUDs, or asked their husbands to, some even triumphantly posting pictures of the devices they say almost ruined their lives.
One of the groups welcomes its more than 7,000 members with a pinned post that assures them they are not alone and that healthcare professionals might dismiss their side effects but they must fight for their right to healthcare.
Most women in these groups have the Mirena, a popular brand of hormonal IUD which is inserted into your uterus where it releases a small amount of progestin (a synthetic version of the naturally-occurring hormone, progesterone) which thickens the cervical mucus, making it a hostile environment for sperm so they can't reach the egg.
There have been around a million Mirenas inserted over the past 10 years in Australia and while there have been just 754 adverse effect reports to the Therapeutic Goods Administration, of which 205 were pregnancy-related reports, these Facebook groups are constant streams of horror stories.
Australia’s major hospital, healthcare and family planning organisations are united in calling for increased access to IUDs and last year when a Queensland woman nearly bled to death after her Mirena perforated her uterus, Australian doctors defended the devices and as they did when the ABC aired a segment on the possible adverse side effects of the devices.
BuzzFeed News asked five Australian reproductive healthcare specialists to respond to some of the most common concerns voiced by women in these groups.
Self removal
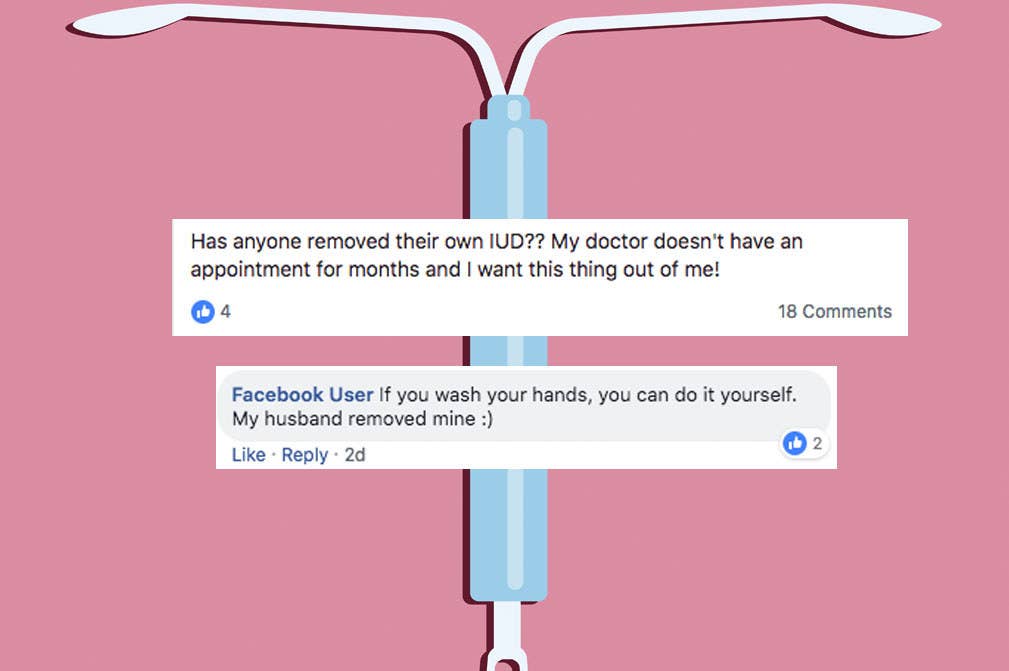
Family Planning NSW medical director Dr Deborah Bateson said while removing an IUD in a doctor’s surgery is usually straightforward, “even more so than the insertion”, it isn’t something doctors recommend doing at home.
“It still requires training, specialised equipment including a speculum to visualise the cervix and special forceps to grasp the IUD threads as well as a good understanding of anatomy and considerable experience in knowing which way to pull depending on the position of the uterus and when to stop if things aren’t going according to plan," Bateson, who is a practicing gynaecologist, told BuzzFeed News.
Dr Catriona Melville is the deputy medical director of Marie Stopes Australia, a national abortion, vasectomy and contraception provider, said only a trained healthcare professional should remove an IUD.
“Occasionally women can have a vasovagal or ‘fainting response’ to the device passing through the cervical canal,” Melville told BuzzFeed News. “This is easily managed in a clinical setting but could pose a risk at home.”
Melville added that if a woman removed the device in the seven days after she had had sex without any other contraception, there was a “risk of pregnancy from that episode of sex” and she might need to take emergency contraception.
Weight Gain

Many women say they have gained weight since getting their IUD inexplicably or because they feel too fatigued and sick to exercise.
Melbourne obstetrician gynaecologist and fertility specialist Dr Melissa Cameron said weight gains on the hormonal IUD are “fairly minor” and “major gains are rare”.
“Many women will notice an initial increase in weight (mostly due to fluid retention) but this usually evens itself out within the first few months after insertion," Cameron told BuzzFeed News.
Sydney specialist obstetrician gynaecologist Dr Talat Uppal said less than 5% who use the Mirena had substantiated weight gain and the overall weight gain was “minimal”.
“You have to analyse the weight gain in the context of ageing and other dietary and exercise interactions,” Uppal, who is also a senior clinical lecturer at the University of Sydney, told BuzzFeed News.
Bateson and Melville both also pointed out that weight gain tended to affect women as they got older.
Mental health

Hundreds of women report the devices caused not only mood swings but in many cases depression, anxiety, panic attacks and even obsessive compulsive disorder or depersonalisation. Some of the women have admitted they did have preexisting mental health conditions but believe the device has exacerbated it.
Specialist obstetrician and gynaecologist Dr Pathma Edge said it was a possible side effect but it was a “very low dose” of hormones going “directly to the uterus” so mental health side effects were less common than the oral contraceptive pill.
"Most doctors should mention the possibility of mood swings in the same way that they should with any hormonal treatment but it is less common with the Mirena," Edge, who is also a clinical senior lecturer at the University of Western Australia, told BuzzFeed News.
Cameron said she warns all of her patients about the potential impacts a hormonal IUD can have on mental health, “particularly women who have had prior mental health conditions”.
“From my clinical experience the most common reports are of increased irritability and mood lability, tending to depression,” she said.
“I have had a few patients have significant, debilitating changes, necessitating removal of the Mirena [and their symptoms resolved].
“Again these effects are mostly temporary and improve with time.”
Melville referred to a 2018 research from Ohio State University published in Contraception Journal which found there was not an association between depression and hormonal IUDs.
“There is no clear evidence that progestin-only contraception causes, worsens or improves depression,” she said.
“Some women do report mood changes during use of hormonal contraception, but in studies mood changes are also reported by women who are not using hormonal contraception.”
Bleeding
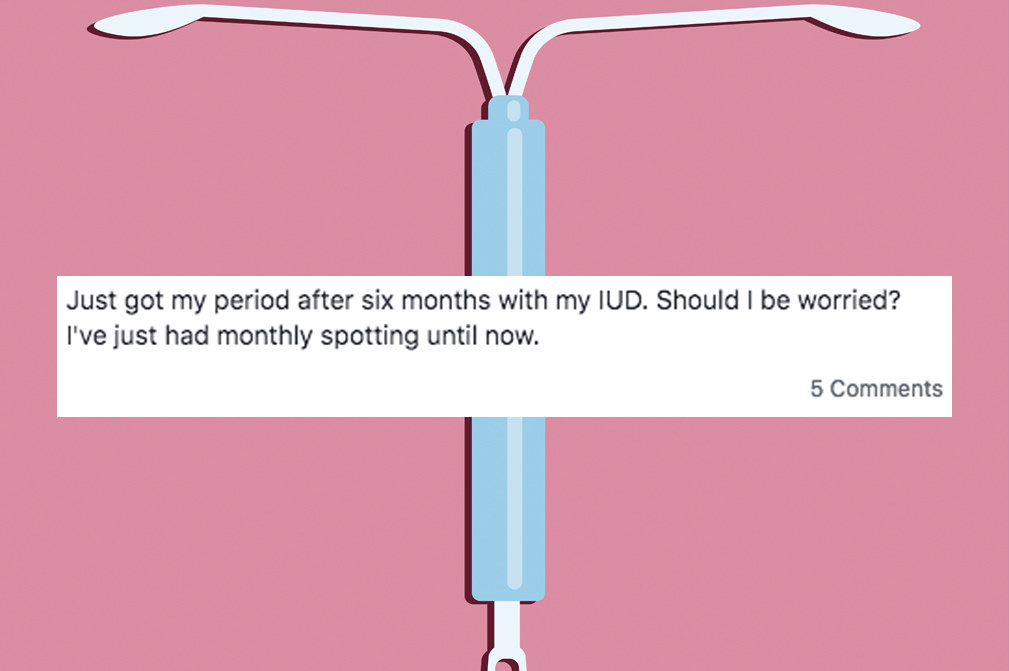
Women in the groups report varying levels of spotting (bleeding lightly) or menstruating heavily and are worried particularly when they get a random period a few months or even years into having an IUD.
Melville said some women will have normal bleeding patterns after insertion but some will experience longer and more frequent bleeding.
“This is more common in the first three to six months after insertion and often settles with time,” she said. “Irregular bleeding may be present in around one in five women at one-year of use.”
If a patient is worrying about bleeding they should seek medical advice to rule out sexually transmitted infections, she said.
Cameron said bleeding can happen particularly when a Mirena is getting closer to the five-year expiry date.
“If the bleeding is unusually heavy or painful or prolonged she should see a doctor to exclude pregnancy or infection,” she said.
Other side effects
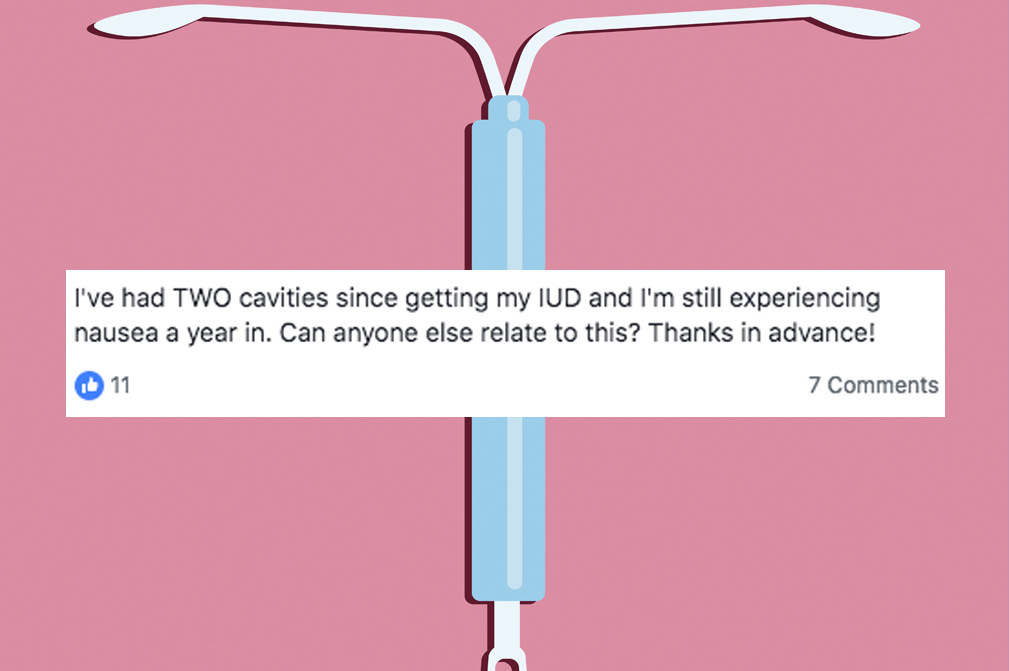
There are a multitude of other side effects reported in the Facebook groups including dental problems (including cavities), hypothyroidism (an underactive thyroid gland), heartburn, cystic acne, hair loss, back pain, bloating and nausea.
Edge said the IUD is not responsible for dental problems, hypothyroidism, reflux, heartburn, indigestion and it was “very unlikely” to be the cause of cystic acne, hair loss and nausea.
If placed properly it does not cause back pain but patients could request a scan to check the device is in the right position, she said.
Bateson said hair loss is an uncommon but potential side-effect of the Mirena, occurring between 1 in a 1000 to less than 1 in 100 women and is listed in the product information. She confirmed there was no evidence the devices caused dental problems, hypothyroidism, reflux, heartburn and indigestion.
Bateson said all hormonal contraception could be associated with hormonal side-effects and although the hormonal IUD had a very low dose of progestogen, “which mainly acts locally in the uterus”, some women may be “very sensitive to even the smallest dose of hormones while others experience no side effects”.
“Knowing which side effects are more common and which are very rare is useful information prior to getting an IUD,” she said.
Unlike the combined hormonal contraceptive pill which contains oestrogen and can be used to improve acne, Bateson said, the hormonal IUD can be associated with new onset acne or worsening acne including a possibility of cystic acne for a small proportion of women.
Nausea and bloating are recognised as uncommon side-effects of all hormonal contraception, she said, but should settle after the first few months.
“The manufacturer’s information will list every symptom that women encountered during initial studies and pharmaceutical trials of the method but this doesn’t mean that the IUD itself caused those symptoms,” Melville said.
“Within one month of insertion of the hormonal IUD, the progestogen hormone released in the uterus, or endometrium, thins its lining and even less hormone will then be absorbed into the bloodstream.”
She said studies have shown that the rate at which women stop using the hormonal IUD due to side effects is not significantly different from those stopping the copper IUD which has no hormones and “therefore it cannot be the cause of the hormonal symptoms described”.
Uppal said it was important not to trivialise the experiences of women but that patients needed to weigh up the benefits of their contraception and the side effects against the reality of an unplanned pregnancy.
“We are trying so hard to build up long-acting reversible contraceptive (LARC) use because Australia is so behind other [Organisation for Economic Co-operation and Development] countries,” she said.
“Almost all forms of contraception have side effects and those that don’t have much higher failure rates so it is actually amazing how LARC efficacy is similar to irreversible methods like a vasectomy and sterilisation.
“The great thing about IUDs is you can always have them removed.”
The Crash

A topic that generates ongoing discussion in these groups is what they call "the crash". This is the idea that once the IUD is finally removed the side effects actually increase in severity. These changes in mental and physical health are caused by a “drop” in hormones now the device is gone, Facebook users say.
All five experts interviewed by BuzzFeed News said “the crash” was not validated by research.
Edge said: “This is not a real phenomenon.”
Uppal said in her more than 20 years of clinical practice she has never seen a patient who has complained of “the crash”.
“We are only as good as the literature we have in front of us and the literature so far has not shown there is any kind of mental or physical falling apart crash after removal that I’m aware of,” Uppal said.
Bateson said the “so-called IUD crash” was not backed up by scientific evidence.
“While removal of a hormonal IUD will result in changes including periods reverting to their previous pattern before the IUD was inserted – which for some women may mean they become heavier and more painful again – there is no scientific evidence that a drop in the level of progestogen hormone causes negative symptoms,” she said, adding the dose of hormones was lower than other hormonal contraceptives.
Melville said "the crash" was not reported in medical or scientific literature and there wasn’t a plausible biological explanation.
The hormonal IUD has little effect on what is called the hypothalamic-pituitary ovarian axis (hormonal pathways between the brain and the ovaries) and and estradiol (estrogen) concentrations in the blood are not reduced, she said.
“Additionally, the majority (75%) of women continue to ovulate when using [an IUD],” Melville said.
“Once a hormonal IUD is removed any local hormonal effect quickly disappears and there is no evidence of delay in a return to ovulation and fertility.”
Pregnancy concerns
Women experiencing breast tenderness, nausea and bloating are concerned about having fallen pregnant on the IUD despite, in some cases multiple, negative pregnancy tests.
“The hormonal IUD is 99.8% effective at preventing pregnancy and is a highly effective method of contraception,” Melville said.
“It doesn’t rely on you remembering to take a pill every day so there is no failure due to human error.”
Cameron said: “The failure rate is around 0.2% for the first year and over five years 0.7% to 1% so essentially it is a very effective form of contraception, more effective than the pill.”
Edge added: “No contraceptive, even a tubal ligation is 100% effective.”
Fertility concerns
After having the device removed, women have turned to the groups to find out how soon they are likely to conceive as dozens of Facebook users claim they have fertility issues even after the device is removed.
“The idea that an IUD can make you infertile is an old, but very persistent myth,” Melville said.
“It probably stems from the days when STIs went undetected and these caused pelvic infection.”
Return of fertility after intrauterine contraception use was similar to fertility rates after stopping oral contraceptives, she said, adding that removing the device before, or during, a menstrual cycle meant a woman should “theoretically be able to conceive within seven to 12 days” during her next ovulation.
“Often women don’t realise they had a pre-existing fertility problem and only notice when they stop a contraceptive method and try to conceive,” Melville said.
“The contraceptive hasn’t caused the fertility issue – the issue has just been ‘hidden’ while the method was being used.”
Cameron said the IUD can in some cases help fertility as it can slow down or reduce the growth of endometriosis and adenomyosis (both of which can negatively impact fertility).
“The exception is if pelvic infection occurs - either from insertion of the IUD which is very rare or sexually acquired when women who change from condom use for contraception to only IUD may increase their risk of exposure to STIs.”
Bateson said a number of studies have shown no association between IUD use and a reduction in future fertility and there is no evidence of a delay in the return to fertility immediately on removing an IUD.
“The pregnancy rate for women one year after removal of a hormonal IUD is the same as it is for women who do not use contraception,” she said.
Partners feeling the IUD
There are many questions about whether male partners should be able to “feel” the IUD during sex and whether anything can be done about it.
“The IUD sits inside the uterus; during intercourse a penis will only be inside the vagina and can’t enter the cervix so if the device is correctly inserted then you and your partner should not be able to feel it,” Melville said.
The strings or threads of the IUD sit outside the cervix and are used for removal of the device and they usually “soften and curl around the cervix” soon after insertion of the IUD.
“However it’s possible your partner may feel these in the few days immediately after insertion,” she said. “Occasionally the threads are a little too long and don’t curl out of the way in which case they can be trimmed by your doctor.”
Uppal said if a patient is really distressed about her partner feeling the strings she will offer to remove the device or cut the strings flush with the cervix.
“But then if the strings are too short there is the potential the woman might have to go into the theatre to a general [anaesthesia] to get it taken out if we can’t get it out with a little device we have which slides into the cervical canal,” she said.
“I’ve cut the strings flush probably two or three times in my career.”
Loss of libido
Edge said the IUD wouldn’t affect libido more than any other hormonal contraceptive.
“Most women have an increased libido due to the fact that they have lighter periods and a safe contraceptive,” she said.
Melville said there was no evidence to support a reduction in libido caused by the device.
“Low libido in women is complex and related to other issues such as mental health problems and stress,” she said.
