This year has barely started, and already 400 food products — from sandwiches, salads, yogurt, and wraps to ready-to-eat breakfast foods — have been recalled due to potential contamination with Listeria bacteria.
The recalls were all linked to one company, Fresh Ideation Food Group, which said that the products were sold in nine states from Jan. 24 to Jan. 30.
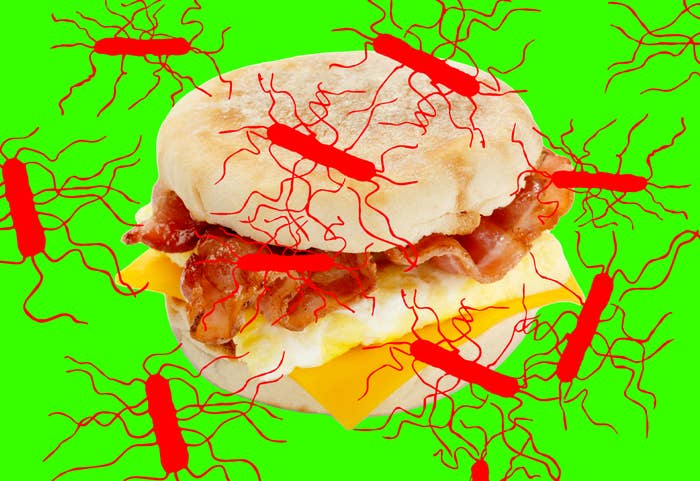
Thankfully they haven’t made anyone sick, and the Food and Drug Administration posted a list of the contaminated products in early February. The recall included bacon, egg, and cheese sandwiches; blueberry and banana chocolate chip muffins; and finger sandwiches made with ham, chicken salad, or tuna salad. They were sold in a variety of stores and vending machines, and often marketed to travelers. (The products have a "fresh through" or "sell through" date ranging from Jan. 31 to Feb. 6 and most have a “Fresh Creative Cuisine” label.)
While that was the most recent Listeria monocytogenes outbreak, there will likely be more this year.
Every year, about 1,600 people get sick from a Listeria infection, known as listeriosis, and around 30% who get it die. That makes Listeria the third-leading cause of death from foodborne illness in the United States.
This type of bacteria is more likely to cause serious infections in young children and people who are pregnant (it can cause miscarriages and fetal death), have a weakened immune system, or are over the age of 65.
Symptoms of a Listeria infection typically begin around two weeks after you encounter the bacteria; the germ can cause many health problems, from mild stomach upset to severe blood and central nervous system infections.
Healthy people are less likely to develop invasive infections like these, and are more likely to have symptoms like diarrhea and fever. However, the symptoms can include fever, muscle aches, headache, stiff neck, confusion, loss of balance, and seizures. People with invasive illnesses are typically treated with antibiotics, although most people recover from a Listeria infection without antibiotic treatment.
Here’s what experts recommend you know to avoid getting sick and the steps you can take to safely store food and drinks.
What is Listeria, and how does it get into food?
Listeria is unlike other types of germs because it can grow well at the low temperatures found in a refrigerator and even survive in the freezer as well.
The germs are widely distributed in food processing environments. They can multiply and ultimately make you sick due to ineffective cleaning and sanitation, poor conditions of equipment, and low-humidity or low-oxygen environments in food.
“Many food manufacturers who make ready-to-eat food products are constantly in search of Listeria species in their manufacturing plant that may come in on raw ingredients or be found in the processing environment to assure it is not being harbored where it can cross-contaminate other products,” Faith Critzer, an associate professor at the University of Georgia Department of Food Science and Technology, told BuzzFeed News.
Once Listeria is found, it can be difficult to remove because of its ability to survive and grow in colder temperatures.
Ellen Shumaker, the director of outreach and extension for Safe Plates food safety program at North Carolina State University, told BuzzFeed News that temperature control is important to prevent bacterial growth. She suggested using a thermometer to check the temperature; the FDA recommends keeping the refrigerator at or below 40 degrees, which slows the growth of the bacteria, and the freezer at 0 degrees, which stops its growth but doesn’t kill it.
The FDA also recommends sanitizing places where food is stored or prepared, including the inside walls and shelves of the fridge, cutting boards and countertops, and utensils.
“Other steps that people can do to reduce their risk of Listeria and other foodborne illness is to use a food thermometer when cooking meat, poultry, and egg products, wash hands before handling food and after handling raw foods, and to reduce time that hot foods or cold foods sit out at room temperature (put away before four hours),” Shumaker said.
Additionally, Critzer recommends heating up ready-to-eat food to 165 degrees before consumption, which can kill the bacteria.
“While there are nuances to different recommended safe cooking temperatures for different types of products, this temperature is uniformly recognized as one which would be sufficient to inactivate Listeria monocytogenes if it were present,” she said. “Tip-sensitive thermometers offer an easy way to check the temperature of foods so you know you’ve hit the mark.”
Here are foods and drinks more likely to have Listeria
Outbreaks are often associated with unpasteurized milks and cheeses, ice cream, deli meats, and raw or processed vegetables and fruits.
The last outbreak of 2022 included enoki mushrooms, which resulted in three hospitalizations but no deaths. Deli meats and cheeses, Brie and Camembert cheese, and ice cream were also the source of outbreaks in 2022.
People at high risk of serious infection are often told to stay clear of soft cheeses, unpasteurized milk, raw fruits and vegetables, and lunch meats and cold cuts.
Here’s what to know and how to store products to help avoid infection.
Unpasteurized milk
States can place their own regulations on unpasteurized milk production and distribution. However, several states prohibit the sale of raw milk for consumption due to dangerous bacteria that can cause health risks, such as Salmonella, E.coli, Campylobacter, and Listeria.
If you drink unpasteurized milk, you should know it’s estimated to be 50 to 160 times more likely to cause a Listeria infection compared to when produced with pasteurized milk — making it the riskiest product to eat or drink. Unpasteurized milk products, including soft cheeses, ice cream, and yogurts, also have a greater chance of making you sick.
The CDC recommends checking labels on milk products and making sure they say, “made with pasteurized milk.” However, pasteurized milk can also become contaminated as a result of unsanitary conditions when processed.
Raw fruits and vegetables
One of the US’s most severe Listeria outbreaks was from contaminated cantaloupes, which led to 143 hospitalizations and 33 deaths in 2011. Since then, outbreaks have been linked to caramel apples, stone fruits, and minimally processed vegetables.
Outbreaks associated with fresh produce, including fruits and vegetables, begin with the crop-growing environment, processing, and retailing. The soil, water, storage, and roads and urban development are places where Listeria has been documented during produce production.
Lunch meats and cold cuts
In deli meats, including cold cuts, lunch meats, hot dogs, and pâtés, Listeria can easily spread among food on countertops, deli slicers, surfaces, and hands. Listeria outbreaks have been linked to fully cooked chicken, deli-sliced items, and pork and ham products.
The CDC recommends separating meats from other foods, utensils, and food surfaces. Additionally, washing your hands before and after preparing food is important in protecting against infection.
To safely store products, deli meats should be sealed and unopened for no more than two weeks in the fridge. For opened products, products should not be stored in the fridge for more than three to five days.
Who’s at risk
People who are pregnant
Listeria infections are 10 times more likely to affect pregnant people than other healthy adults.
It can be passed to fetuses and newborns by spreading through the placenta. If infection occurs, it can cause miscarriages, stillbirths, and newborn deaths. According to the CDC, an outbreak of Listeria in queso fresco in 1985 made 142 people sick and caused 20 miscarriages. Overall, 18 adults and 10 newborns died during the outbreak.
According to the American College of Obstetricians and Gynecologists, many pregnant people who have listeriosis do not have symptoms. The infection can still pass to the fetus whether or not a person has symptoms.
People who are 65 and older or who have a weakened immune system
More than half of people who have a Listeria infection are over the age of 65, and are four times more likely to get infections compared to other younger adults. Additionally, people 65 and older are more at risk of being hospitalized from foodborne illnesses due to changes in the body, including the immune system.
People with weakened immune systems due to medical conditions, such as cancer, diabetes, liver or kidney disease, alcoholism, and HIV or AIDS, are more likely to get a Listeria infection. Additionally, immune system–suppressing treatments such as steroids or chemotherapy can make it more difficult to fight the infection.
If you do think you consumed a product that may have been contaminated with Listeria, it’s important you reach out to your doctor or healthcare provider if you start experiencing symptoms. ●
