
A dangerous HIV outbreak in Charleston, West Virginia, will require “low-barrier” needle exchanges to stop the disease from spreading, according to a preliminary CDC investigation obtained by BuzzFeed News.
The only problem is that new state and city laws banned those needle exchanges in April.
The CDC’s investigation into the HIV outbreak in Charleston comes as the city of 48,000 has emerged as the fiercest battleground in a nationwide reckoning over syringe exchanges, long shown to stop HIV outbreaks among people who use drugs. Needle exchange locations have recently faced shut down efforts in Indiana, California, and New Jersey, despite fears of more HIV outbreaks amid a nationwide epidemic of injection drug use.
“It's history repeating itself,” said Beth Connolly, substance use prevention and treatment initiative director at the Pew Charitable Trust and the former commissioner of New Jersey’s Department of Human Services. Despite decades of evidence that needle exchanges work to stop HIV and hepatitis outbreaks in addition to helping people enter recovery programs, she said, “we still are here in 2021, and people are still trying to get rid of syringe services programs.”
In February, CDC's HIV prevention chief (now temporarily assigned to the agency's COVID-19 response) Demetre Daskalakis urged the Charleston city council to consider syringe exchange programs, calling the city’s HIV outbreak the “most concerning” one nationwide. Largely spreading among people who inject illicit drugs, it now stands at 68 cases in the last year, with many more cases expected to turn up with more testing.
At a presentation last week, CDC experts reported preliminary results of an investigation into the outbreak during a closed-door meeting with state and local health officials. Reporters and members of the local HIV Task Force were excluded from the presentation, a move that was viewed by some as wanting to keep the polarizing topic under wraps.
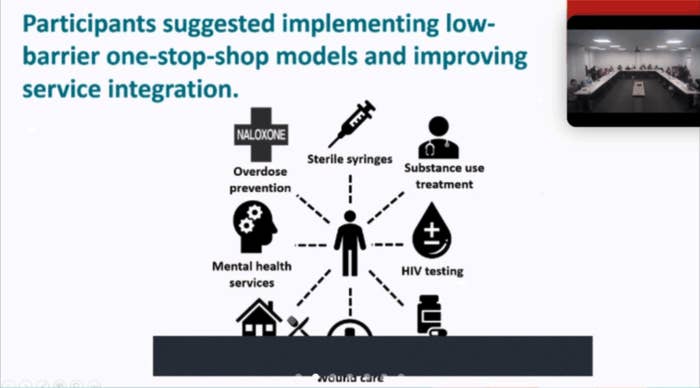
BuzzFeed News obtained the CDC’s presentation slides and a recording of the two-hour meeting, showing that the CDC “Epidemiologic Assistance” team found widespread mistrust of hospitals among people who use drugs and a lack of HIV testing in emergency room and clinic settings. Both people who use drugs and health officials interviewed by the federal health agency called for "low-barrier” one-stop combinations of syringe services, medical care, and HIV testing to stop the outbreak from growing.
"The most commonly mentioned suggestion from both people who inject and stakeholders about how to improve access to services and service integration was to implement this one-stop model," a CDC presenter said during the meeting. About a third of the people with HIV surveyed said they did not have housing and the same number reported recent arrests. Half said they injected drugs more than once daily, typically heroin or fentanyl, and around 15% reported doing sex work, raising the risk of sexual transmission of HIV.
“CDC is in large part telling us what we already know, which is that people need access to sterile syringes,” said West Virginia University epidemiologist Robin Pollini, who reviewed the slides for BuzzFeed News. “There's a lot of suffering documented in this presentation.”
Interviews with both people who inject drugs and medical staff found stigma and mistreatment were commonly encountered in healthcare settings. “I wouldn’t go to another hospital unless I was dying,” one man told the CDC investigators. “Because they don’t care about you.”
The report noted that none of the 65 HIV patients interviewed were prescribed pre-exposure prophylaxis (PrEP) before their diagnosis, despite multiple earlier visits to hospitals for wounds and illnesses caused by injection drug use. “You have to have a negative HIV test before you can go on PrEP, and they aren’t bothering to do the testing in the first place,” said Judith Feinberg, an infectious disease expert at West Virginia University.
According to the CDC representatives at the meeting, the investigation is ongoing and a final CDC report is expected in August. The agency referred a request for comment from BuzzFeed News to West Virginia’s health agency.
“Stopping HIV in West Virginia and in Kanawha County is the right thing to do and will save lives, resources and money,” Andrea Lannom of the West Virginia Department of Health and Human Resources Bureau for Public Health told BuzzFeed News by email. She did not respond directly to questions about the low-barrier syringe service recommendation, but said communities can work on making sure “services are available to meet people where they are.”
But meeting people where they are will continue to be a problem in West Virginia. In April, the state passed a law, SB334, aimed at dismantling most needle exchanges operating in the state. The law killed off a grassroots program in Charleston called SOAR, which had started offering needle exchanges and HIV testing in the last two years after the contentious shutdown of the city's own syringe service in 2018. SOAR was the first group to ring alarm bells over the city’s HIV outbreak in late 2019, after tests by medical volunteers at its bimonthly health fairs turned up eight positive cases.
The CDC findings are “disheartening, but also validating, to find you were doing exactly what needs to happen,” SOAR president Sarah Stone told BuzzFeed News. “But also, it’s frustrating, because we may be the small handful of people here that believe that to be true.”

Among other restrictions, the new state law requires labeling syringes — which would link needles to the individuals who used them — and mandates state licensing and approval from county politicians to operate. Against CDC recommendations, the law also requires that exchanges try to match the number of needles handed out with the number of returns and only give needles to people with state-issued identification, discouraging people experiencing homelessness or people using illicit drugs who fear being arrested from participating. It also forbids people from picking up needles for others, which can be helpful in a rural state with limited public transportation.
“We're in the middle of an HIV crisis, and people don't know because we're not talking about it. We're talking about needles, and we're talking about homelessness, we're talking about vagrants, and we're not talking about people,” said Stone. “We're talking about the annoyances of people that use drugs, and that's not right.”
The ACLU won a temporary injunction against the state law on Monday. While the law was set to go into effect on July 9, it has already effectively stopped SOAR’s health fairs, which depend on volunteers to operate. “We had nurses, and med students, and physicians, at each of our health fairs, who are now scared to set up a health fair with us,” said Joe Solomon, another one of SOAR’s leaders. “Because they're afraid they'll leave in handcuffs.”
A smaller needle exchange that requires identification and return of labeled needles on the east side of the city abides by the new state law but is what the CDC presentation described as a “high-barrier” needle exchange. Another barrier is that the majority of the people who use drugs interviewed by the CDC live across the Kanawha River on the city’s western side.
The current HIV outbreak in Charleston was predicted by a 2019 Johns Hopkins University study that looked at the closure of its city-run needle exchange site. City officials condemned its findings, calling exchanges “addiction empowerment,” and complaining that the researchers only interviewed people who use drugs. "If we do see a disease progression into our community, being high rates of HIV or other things, we may have to have the discussion again, but right now, no,” Kanawha-Charleston Health Department chief Sherri Young told a local news station in May 2019.
This week, Young announced she was resigning from her position.
UPDATE
This story has been updated to clarify that CDC's Demetre Daskalakis has been temporarily assigned to the agency's COVID-19 response.
