
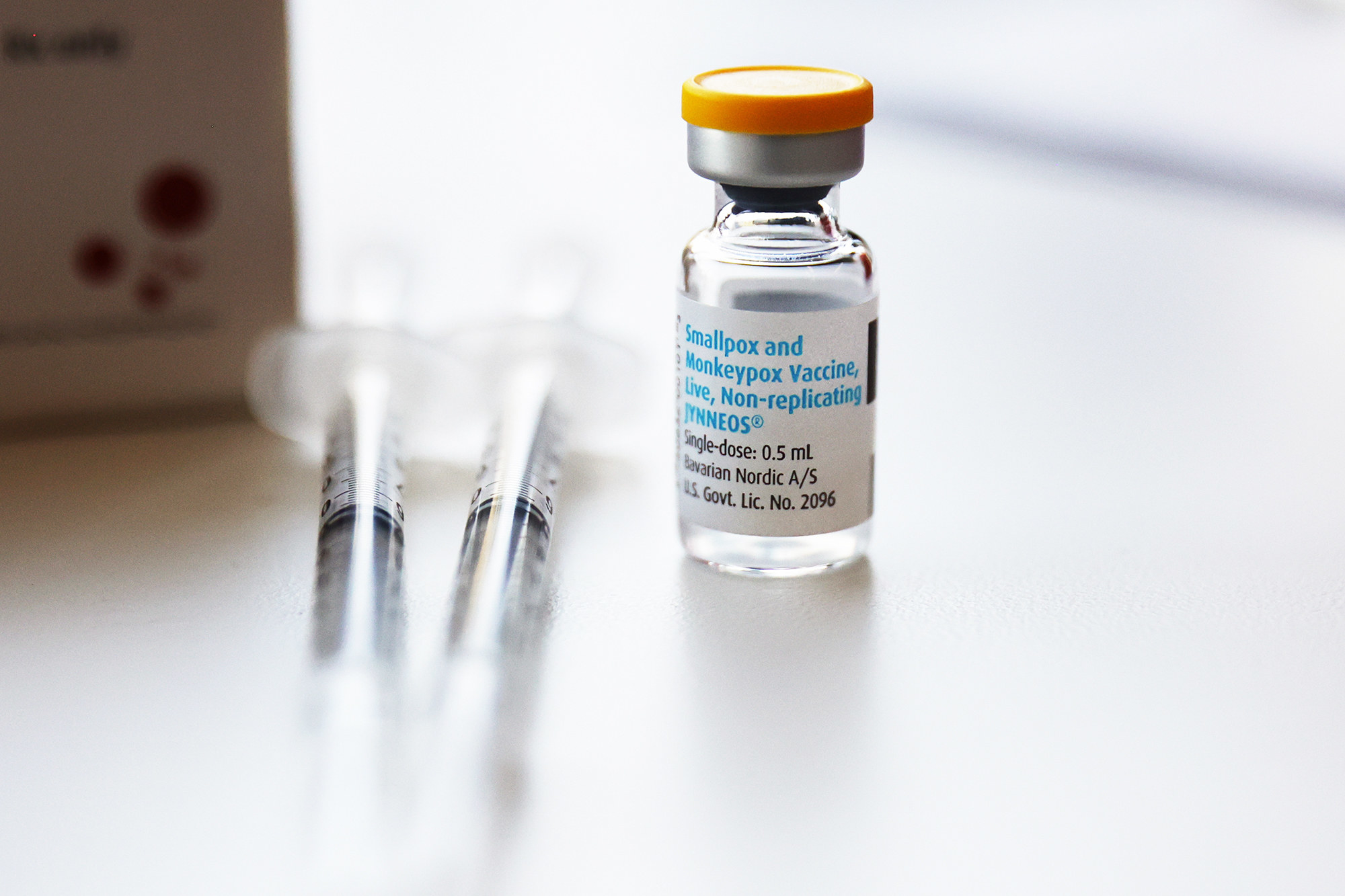
In an effort to stretch the limited supply of monkeypox vaccine, US health officials announced this week that they will allow people to get “intradermal” vaccinations, or doses injected directly under the top layer of skin.
This means one dose can now be used to inoculate five people. The strategy required an FDA emergency use authorization, which also allowed for high-risk children to be vaccinated as well.
Typically, the approved Jynneos vaccine is injected into the deeper fatty tissue (subcutaneously), and then a second shot is given four weeks later. In other words, it usually takes two doses over a month to achieve immunity, which can help control the outbreak.
Jynneos shots can be given before or after exposure to stop the monkeypox virus and are considered the best way to prevent infection or symptoms that can include fever, headache, fatigue, rash, and raised lesions.
“[Vaccines] are the preferred way to treat monkeypox,” said Dr. Amesh Adalja, senior scholar at the Center for Health Security at the Johns Hopkins Bloomberg School of Public Health. “They confer immunity into the at-risk population.”
As of Aug. 11, there have been 10,768 reported cases of monkeypox in the US. This is likely an undercount, said Dr. William Schaffner, an infectious disease specialist with Vanderbilt University Medical Center in Nashville.
In early August, the Biden administration declared the current wave of monkeypox cases a public health emergency, which opened the door for more resources, including vaccinations.
The Department of Health and Human Services says it has secured 1.1 million doses and has shipped more than 620,000 doses of Jynneos to states and jurisdictions so far. However, an additional 150,000 doses won’t arrive in the US until September, and the rest of the doses may not be available until 2023.
The current supply of Jynneos, if given at two doses a person, can cover only about a third of the estimated 1.6 million queer men in the US who should be vaccinated, according to the Washington Post. That leaves about 1 million people to wait months before they become fully vaccinated.
“We sure could use a heck of a lot more vaccine,” Schaffner said.
Here’s how officials are stretching vaccine supplies to handle a rapidly expanding case count and what we know about the ability of the vaccine to protect you when given intradermally or subcutaneously.
What are intradermal injections?
These injections involve inserting the needle right under the skin’s top layer, which produces a small bubble on the surface that may leave a scar. The method provides more of an immune response than subcutaneous vaccinations that poke deeper into the fatty layer under the skin, Adalja said.
In practice, using the intradermal method means only one-fifth of a regular dose is needed. So why aren’t all vaccines administered in this way?
“We sure could use a heck of a lot more vaccine,” Schaffner said.
The intradermal route requires a very fine needle and some specialized training. Some healthcare providers are familiar with the method as it’s used for the tuberculosis skin test. In that case, tuberculin, a purified protein, is injected under the skin, which can trigger a swelling that is considered a positive TB test.
Research indicates that intradermal administration is a safe and effective vaccination method for rabies, influenza, and the hepatitis B virus.
There’s not a lot of data proving the effectiveness of the monkeypox vaccine when given intradermally. Some preliminary studies have shown it's about as protective as the traditional subcutaneous injections, Adalja said.
The main issue is in the actual delivery of the vaccine, Schaffner said. “It’s an art form,” he said. “It’s so much more difficult to do correctly each and every time.” Providers need to be specially trained; if nurses who are familiar with doing TB tests are brought out of retirement to help, they need to have the correct licensure to avoid liability.
The FDA has been getting questions from pharmacists about how many times they can use a vial and how long someone should wait before the second shot, which Schaffner believes the FDA can answer.
Will stretching monkeypox vaccines in general work?
The CDC says that the intradermal method should be as effective as a regular shot, pointing to a 2015 study that found that intradermal influenza vaccines in men with HIV were as effective as intramuscular flu vaccines. Another study that looked specifically at the Jynneos monkeypox vaccine found similar immune responses between the intradermal and subcutaneous administrations.
Some cities, including New York City and Washington, DC, have already been administering only one subcutaneous dose of the Jynneos vaccine and waiting for more supplies before administering the second shot.
Although the highest level of antibody immunity comes after the second dose, this approach allows more people to potentially build at least partial immunity, said Dr. Cesar A. Arias, chief of the infectious disease division at Houston Methodist Hospital.
Exactly how much immunity, no one can say, but it seems unlikely that delaying the second dose will affect overall protection once you get the second shot, Schaffner said.
Administering a single subcutaneous shot is “a very reasonable scientific plan at this point in time,” said Dr. Aaron Glatt, a spokesperson for the Infectious Diseases Society of America and chair of medicine at Mount Sinai South Nassau.
Why is there a vaccine shortage?
There are actually two monkeypox vaccines available in the US, said Arias, who is also codirector of the Center for Infectious Diseases Research at the Houston Methodist Research Institute.
Although the US at one point had millions of doses of the Jynneos vaccine, the only one fully approved by the FDA, the “doses have a limited shelf life and can no longer be used,” said Dr. Mark Loafman, a board-certified family physician with Cook County Health in Illinois.
A second product, the ACAM2000 smallpox vaccine, can be used for monkeypox in certain people under the FDA’s expanded access protocol for so-called investigational new drugs.
“It’s known to be effective against monkeypox but was not licensed for that use,” Loafman said. Although the ACAM2000 vaccine has the advantage of being a single dose, it’s not safe for pregnant people or people with weakened immune systems, eczema, and other skin conditions.
People with weakened immune systems need to get the larger dose, as there isn't enough data on how they react to intradermal delivery, Schaffner said.
It is difficult to administer the vaccine for older people who have thin skin as a result of certain skin conditions. “It’s easier to go through the skin and, if the skin is very thin, it may not contain the fluid and it leaks out,” Schaffner said.
The side effects are similar with both Jynneos vaccine administration methods, although you can have more redness and itching with intradermal vaccines, and once it heals up there may be some discoloration, Schaffner said.
The 2016 clinical trial comparing the two methods found that intradermal administration resulted in “some mild to moderate side effects like redness, firmness, itchiness, and swelling at the injection site,” FDA Commissioner Robert Califf said at a press briefing this week. “These were all manageable.”
Are only certain people eligible to get vaccines now?
Yes. Until more supplies become available, public health authorities are only giving monkeypox vaccines to those who have had direct close contact with a known or suspected case in the past two weeks or have had multiple sex partners in the past two weeks in an area with known cases as well as a small group of laboratory and healthcare workers who have had direct exposure to the virus, Loafman said.
The virus is primarily spread through close physical contact, including sex, and most US cases have been seen among men who have sex with men. While the virus is certain to spread to other populations, at the moment the focus is on limiting the spread among men who have sex with men and other high-risk communities.
“As more vaccines become available, the eligibility criteria will expand to those with potential exposure risks,” Loafman said.
Do I still need to limit new sex partners if I’ve received one dose of the vaccine either subcutaneously or intradermally?
It’s a good idea to limit new sex partners or even to stay away from shirtless dance gatherings, also known as circuit parties, at the moment if you want to avoid getting monkeypox.
Given that experts don’t know how effective one dose is or when immunity kicks in for a particular individual, “to reduce risk of contracting the virus, it is recommended to avoid any close contact until otherwise approved by a doctor,” Loafman said.
And while the virus is primarily spread by close skin-to-skin contact, it can also be spread, albeit less commonly, by respiratory droplets between two people talking close together, Schaffner said.
Two doses of the monkeypox vaccine are thought to be 85% effective two weeks after the second dose; no one knows how effective one dose is.
“We’re sure it’s not 100%,” Schaffner said.
And the efficacy of the vaccine will vary depending on how long it’s been since your initial exposure to the virus.
“I would advise avoiding sexual contacts at least for three to four weeks, even if the first dose of the vaccine has been administered,” Arias said, adding that waiting even longer is probably better.
“If you have a new partner or even your steady partner, keep the light on long enough so you can inspect each other to make sure you don't have a rash,” Schaffner said. “Then you can turn the light off and have fun.”
The CDC also recommends washing your hands often and avoiding contact with objects that an infected person has used.
Am I protected if I got a smallpox vaccine when I was young?
Routine smallpox vaccinations were discontinued in 1972 because of the worldwide decline in smallpox infections. That means few people under the age of about 50 have had the vaccination, which was about 95% effective, with peak immunity lasting three to five years.
A study dating from 1988 did find that people in Zaire (now the Democratic Republic of Congo) with smallpox vaccination scars had about 85% protection against monkeypox.
“It is very likely that people who received the smallpox vaccine may have some protection, but the majority of those people are older and their immune systems are probably not at their best right now,” Arias said.
Our immune systems naturally decline as we age, which is why older people received COVID boosters before younger groups and why people 65 and over can get a high-dose version of the influenza vaccine.
People who’ve had monkeypox before generally have long-term and often lifelong immunity, Loafman said.
Are there treatments for monkeypox?
Although there are no treatments specifically earmarked for monkeypox, some drugs used for smallpox can help. People with weakened immune systems may benefit from an antiviral drug called tecovirimat (sold under the brand name Tpoxx).
For the most part, monkeypox cases in the current outbreak have not been life-threatening, Glatt said. (Globally, 12 deaths have been recorded so far, among about 32,000 cases.)
“The symptoms tend to resolve by themselves over several weeks so the vast majority of people don’t need treatment,” Schaffner said.
He added, “If you have lesions on your genitalia or in your mouth or inside your rectum, that can be disfiguring and painful, and that’s an indication for treatment.”
