My book How to Be a Patient is about asserting agency during healthcare encounters and navigating the world of modern medicine in a more empowered fashion. If you want to do one thing now to set yourself on this path, the move is to get a solid primary care provider (PCP) — and not any PCP, but one you have chemistry with.
Moving through the world without a PCP places more hurdles between you and the care you’re trying to obtain. It’s more of a hassle, for instance, to go to a specialist (eg. physical therapist, endocrinologist), since many insurance carriers mandate you first have an appointment with your PCP and then get a referral. It also limits your options when you need that prescription from last year refilled, or think you might have strep, or when the discovery of a mole is keeping you up at night.
Today, roughly a third of American patients go without a PCP. Just under half of millennials go without one. Among patients who’ve established primary care, it’s rare for them to see their PCP as a true partner. And yet the research underscores the importance of this alliance. It’s how a provider makes you feel — not merely the information they equip you with — that predicts health outcomes.
The usual responses I get when asking how someone likes their doctor or nurse practitioner go something like:
“Mine is nice enough, but always in a rush.”
“He’s awkward, but supposedly good.”
“I think I’d rather have a woman. Should I see a woman?!”
“When I go to my [provider’s] office, a different person sees me every time. What do you mean, primary care provider?”
On the flip side there is that person who gushes about their provider, telling stories that make you think, Damn, I deserve better. So, onward and upward for the rest of us.
How To Get Started
As you begin to hone your search for a PCP, consider the various types of providers who practice primary care. They include:
- Family medicine physicians
- Internists
- General practitioners (GPs)
- Ob-gyns (obstetrician-gynecologists) and gynecologists
- Nurse practitioners (including family nurse practitioners, primary care nurse practitioners, and women’s health nurse practitioners)
- Physician assistants
- Pediatricians and geriatricians
If you’re coming in cold, the best way to commence the search is by asking providers and nurses you already know and like for a referral. This could be your therapist, your dentist, or a specialist you’ve seen at some point, or an immediate family member’s provider. Next, ask friends and family directly. Finally, do a general search on the internet. Apps like Zocdoc and Healthgrades can help you narrow down choices by reading reviews, but there always seem to be exceptional providers who don’t show up on these sites, either because they keep a low profile, or acquire patients by word of mouth. This is all to say, begin with humans, then move to the web.
Once you’ve compiled a shortlist of people who might fit, the next step is to find out if they’re in network by calling their clinics and asking if the provider accepts your insurance. This is much easier than starting from an insurance network directory online and searching for providers. Often these directories don’t list all the provider’s specialties — for example, one might not list that a family practice doctor also provides maternity care — and the information about whether they are accepting new patients is frequently out of date. Nurse practitioners employed by a physician practice may not be included in directories. Ultimately you’ll get a narrower view of options using this platform.
Once you’ve found people who appear to be a good fit and accept your insurance, cull it down to two or three based on the practice setting, their listed experience, and their location. You can then call the clinic or hospital where they practice, say you’re looking to establish primary care, and ask if the person you’re interested in offers meet-and-greets. Several practices offer them free of charge for potential patients, and several insurance plans cover them for a nominal co-pay. Set up as many as you want.
What To Look For
While the right PCP might look very different from one person to the next, the best ones should possess certain traits. Keep these in mind whether your searching for someone, or reevaluating your current provider. These should really apply to any professional you trust with your body and your health.
They should be willing to explain their thinking to you. If you ask, they should be ready to walk you through how they came to a conclusion—or, better, they should offer this on their own.
They should be curious. Curiosity is a worldview. It propels people toward presence and nimble thinking. Its absence is associated with burnout, ego, and a tendency toward conventionally accepted ideas.
They should be willing to admit when something is outside their wheelhouse. Providers’ not knowing something is more common than patients think, and admitting this is a crucial act of humility that can alter a course of care.
They should be receptive listeners. Pay attention to the way you engage in dialogue with a potential PCP and how they respond to what you say. If your provider consistently decides what is talked about, where the conversation pivots, which questions are dismissed, and when a discussion of a particular item is over, there’s a power imbalance. And this can exist under a guise of charm. The way you talk might seem inconsequential compared to what you talk about, but if there’s a power imbalance exercising your agency will be an uphill battle. A battle you have to ultimately win, because when a provider exerts all the control in a conversation, it increases the risk that they will not get all they need to know from you, making them more liable to take a wrong turn when it comes to your specific needs.
They should be accessible. Ask up front how accessible a potential PCP is:
- If I needed to reach you in a health emergency, how would I go about doing that?
- How much time, on average, are you able to spend face-to-face with a patient?
- What’s the process if I need a prescription, or have a question for you but don’t necessarily need to come in?
You’re looking for potential hurdles here. In other words, what’s between you and this person when you’re out in the world and you need medical help? An operator line? A MyChart message? A full-fledged appointment that must be scheduled and billed as such, even if the problem is minor? Be direct, and look for responses that answer your question rather than skirt it. Think of real predicaments you’ve been in before, where you’ve needed help and run into obstacles trying to get it.
They should speak your language. The PCP you choose doesn’t have to be someone you’d go get beers with, but they should speak your language and have a style and pace that feel comfortable to you.
If you’re sensitive or introverted, look for someone you feel at ease around. Maybe you want an old guard provider, one who’s seen it all from decades of experience; or you might prefer someone freshly graduated with answers to the boards still fresh in their minds. You can find a PCP with additional training in mental health or integrated medicine, if those are relevant for you. Aspects of your identity also factor in—culture, gender, sexual orientation, profession. These are part of your lived life, so you should be able to place them at the table with your PCP.
This is also where the term bedside manner gets tossed around. It’s a phrase we use culturally to excuse bad attitude and poor communication coming our way from medical professionals, and it’s one that has to be retired. To use it is to surrender your agency as a patient, and assume you have to settle for something that doesn’t feel right. A primary care provider who acts without respect and integrity — in a way you can feel — will fail you. The very nature of their role is to meet you where you are and invite ease and trust.
Logistics
The diversity of primary care settings and setups leaves you with a few more things to factor into your decision before you choose a practitioner. Each PCP operates within the confines of a practice setting — some grant them more autonomy and cost you more money, others grant them experience working with a diversity of populations, which can be of equal benefit to you.
Settings
Private practice: These clinics are typically out in the community and run by a group of providers or a single provider who work for themselves.
Community Health Center: These clinics provide care to medically underserved communities and many take patients regardless of their ability to pay.
Hospital system: Large hospital consortiums such as Kaiser Permanente or the Mayo Clinic Health System house primary care divisions.
Teaching hospital: Teaching hospitals on the same campus as medical and nursing schools may house primary care offices or have affiliated primary care clinics offsite in neighboring communities. Massachusetts General Hospital and UCLA Medical Center are examples.
Styles
Traditional Western medicine: This is the prevalent care model in America. Healthcare professionals treat symptoms and diseases using drugs, lifestyle interventions, therapeutic interventions (for example, radiation), or surgery. You may also hear this style called allopathic medicine, conventional medicine, mainstream medicine, or orthodox medicine.
Functional medicine: If the body were a garden bed and its diseases weeds sprouting up, traditional medicine might look to specialists to eradicate the weeds and keep things growing. Functional medicine is more interested in the soil. Providers of this ilk employ a systems approach, meaning that they focus on identifying the root cause of diseases by closely examining patients’ health history and environment.
Integrated/holistic medicine: Practices rooted in this type of care are where you’ll find an emphasis on lifestyle, and an incorporation of Eastern practices such as acupuncture, herbalism, chiropractic care, and massage.
Osteopathic medicine: If you’ve seen a doctor with a “DO” after their name as opposed to “MD,” it stands for “doctor of osteopathic medicine.” Osteopathic medicine focuses on holistic, patient-centered care with a strong foundation in primary care. These providers have additional training in hands-on, manipulative medicine to alleviate pain and restore function to bodily systems.
With these models, more money does not necessarily translate to better care. At the end of the day, primary care is really about the relationship between provider and patient—the setting is secondary.
Ultimately, finding the right PCP takes upfront investment, but it’s at least as important as choosing where to attend college, what company to work for, or where to go on vacation — tasks we greet with more thought and enthusiasm. Channeling your efforts here will pay off, in untold ways, when it comes to navigating the healthcare terrain and getting better care within it. ●
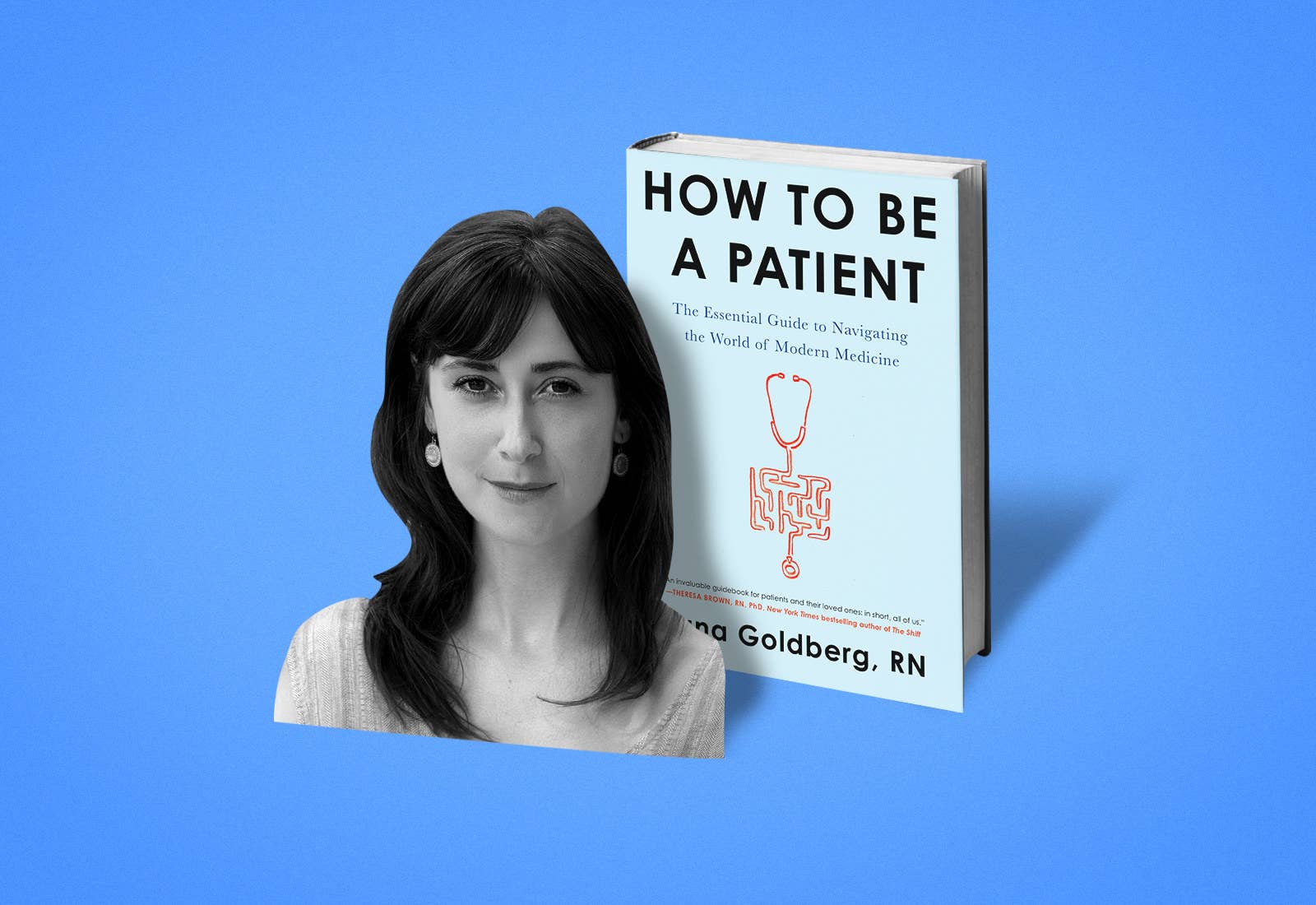
HOW TO BE A PATIENT: The Essential Guide to Navigating the World of Modern Medicine by Sana Goldberg, RN. Copyright © 2019 by Sana Goldberg. To be published on March 19, 2019 by Harper Wave, an imprint of HarperCollins Publishers. Reprinted by permission.
Sana Goldberg, RN, liaises between academia and clinical practice. She has worked with a diversity of patients across settings from the perspective of researcher, social worker, nurse, and provider. An outspoken public health advocate, she’s presented at World Congress, TEDx Harvard, The Society for Neuroscience, and OPHA, with work published in Neuropharmacology, The European Journal of Neuroscience, and forthcoming in the Atlantic. She is the recipient of the Diamond Alumni Award, a member of the International Honor Society of Nursing, and the founder of Nightingale, a movement of story, art, and activism for health equity. She practices in New Haven, CT, while pursuing graduate studies at Yale. How to Be a Patient: The Essential Guide to Navigating the World of Modern Medicine is available March 19.
